ACTH Testing for Safe Steroid Tapering: A Guide to Adrenal Recovery
 Feb, 5 2026
Feb, 5 2026
Steroid Tapering Calculator
Input Parameters
Why This Matters
The ACTH stimulation test measures your adrenal glands' ability to produce cortisol after long-term steroid use. Without this test, doctors can't safely determine when to stop steroids completely. A Mayo Clinic study found that using ACTH testing during steroid tapers reduced adrenal crisis rates from 8.5% to 1.2%.
The HPA axis (hypothalamic-pituitary-adrenal axis) is your body's natural stress response system. Long-term steroid use suppresses this system, which is why careful tapering and monitoring are essential. Stopping steroids abruptly without proper monitoring can lead to dangerous adrenal crises.
Your Safe Tapering Schedule
Note: This calculator is based on guidelines from the Adrenal Insufficiency Coalition (2020) and PJ Nicholoff Protocol. Always work with your endocrinologist for personalized tapering plans.
Why ACTH Testing Matters for Steroid Tapers
Did you know that improper steroid tapering can lead to life-threatening adrenal crises? For patients on long-term steroids, the process of stopping isn't as simple as just quitting. The body's natural cortisol production takes time to restart, and without proper monitoring, serious health risks emerge. A Mayo Clinic study from 2015-2020 found that using ACTH stimulation test during steroid tapers reduced adrenal crisis rates from 8.5% to 1.2%. That’s a dramatic improvement-enough to make this test a critical part of any steroid discontinuation plan.
What Happens During an ACTH Stimulation Test
An ACTH stimulation test is a straightforward procedure where synthetic ACTH (cosyntropin) is injected, and blood samples are taken at 0, 30, and 60 minutes afterward. This test measures how well your adrenal glands respond. A peak cortisol level above 18-20 mcg/dL (500-550 nmol/L) indicates sufficient adrenal function, while levels below 14 mcg/dL (386 nmol/L) show insufficiency requiring continued steroid support during the tapering process.
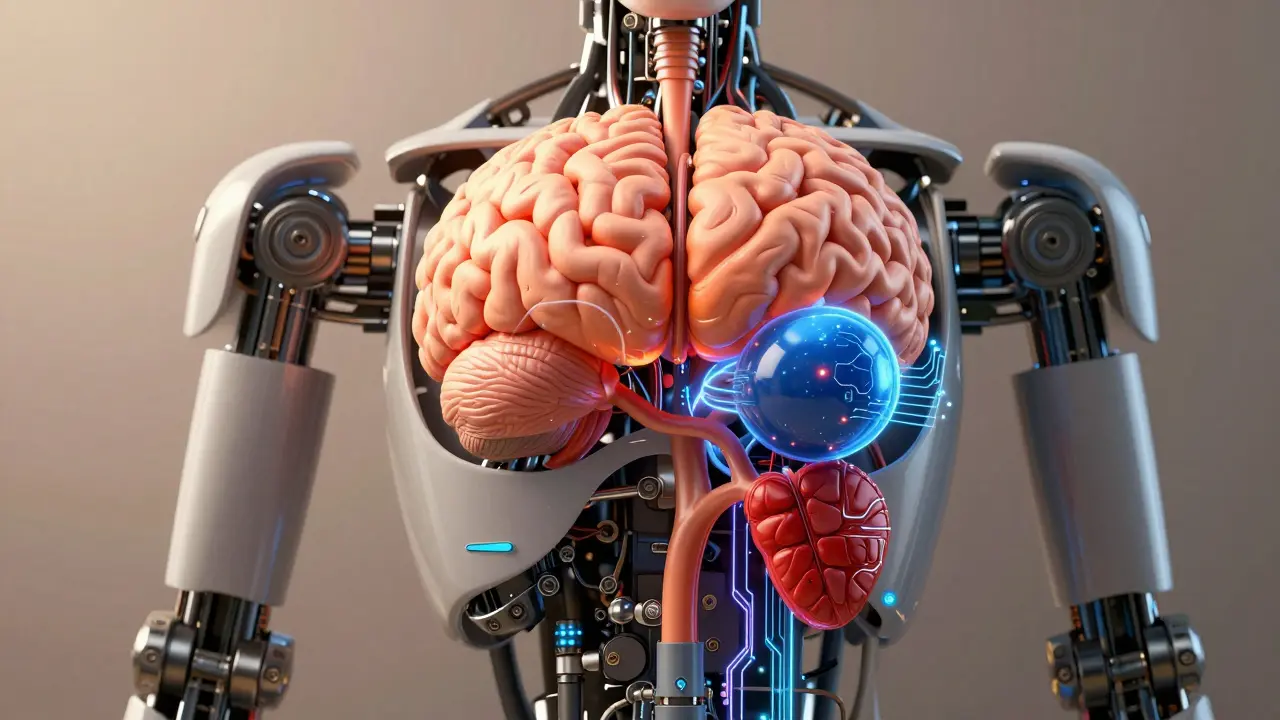
How the HPA Axis Works
The HPA axis (hypothalamic-pituitary-adrenal axis) is your body's natural stress response system. It involves the brain, pituitary gland, and adrenal glands working together to regulate cortisol. Long-term steroid use shuts down this system, which is why careful tapering and testing are essential. When you take glucocorticoid therapy for months or years, your body stops producing its own cortisol. Without proper monitoring, stopping steroids abruptly can leave you without enough cortisol to handle stress, leading to dangerous symptoms like fatigue, nausea, or even shock.
How Steroid Tapers Work Based on Duration of Use
The time it takes to safely taper steroids depends entirely on how long you've been taking them. For treatments lasting 3-12 months, the PJ Nicholoff Protocol recommends reducing prednisone by 2.5-5 mg every 1-2 weeks until reaching a 'triple maintenance' dose of 10-15 mg/day. After that, weekly reductions of 20-25% continue until reaching physiologic replacement doses (4-6 mg prednisone daily). For therapy exceeding 12 months, recovery takes about one month for every month of steroid use. The Adrenal Insufficiency Coalition's 2020 guideline states that patients on long-term steroids may need up to 9-12 months to fully recover adrenal function.
Key Differences Between Current Medical Guidelines
| Guideline | Testing Recommendation | Tapering Speed | Key Focus |
|---|---|---|---|
| Endocrine Society 2024 | Test only for symptoms or high-risk patients | Gradual reduction after reaching physiologic dose | Preventing disease reactivation |
| PJ Nicholoff Protocol | Routine testing at specific stages | Structured 14-step schedule | Duchenne muscular dystrophy-specific |
| Adrenal Insufficiency Coalition 2020 | Testing after 3 months of therapy | 1 month per month of steroid use | Universal monitoring |
Real-World Challenges in Tapering Protocols
Despite clear guidelines, many patients face barriers to ACTH testing. A 2023 survey by the Adrenal Insufficiency Coalition found 61% of patients waited over four weeks for testing, and 23% ended up in emergency rooms due to delays. Rural areas face particular challenges-Dr. Sarah Chen from Massachusetts General Hospital reported that while her hospital reduced adrenal crisis admissions from 12 to 2 per year using structured protocols, rural primary care doctors often struggle to send patients hours away for testing. 'Many don't follow through, leading to dangerous gaps in care,' one rural GP shared on Reddit in June 2024. A 2022 study in Endocrine Practice found 68.3% of primary care physicians felt unprepared to implement ACTH testing due to limited endocrinology access.
What Patients Should Do During Steroid Tapering
Patients can take proactive steps to ensure safe tapering. First, keep a daily log of symptoms like fatigue, nausea, or dizziness. Second, always carry a steroid alert card explaining your need for stress dosing during illness or surgery. Third, schedule ACTH tests before stopping steroids completely. The Endocrine Society's 2024 guideline stresses that testing should occur when patients reach physiologic replacement doses (4-6 mg prednisone) and before full discontinuation. Finally, work closely with your endocrinologist-82% of rheumatologists follow Endocrine Society guidelines, but neurologists managing conditions like Duchenne muscular dystrophy adhere to the PJ Nicholoff Protocol in 95% of cases. For example, if you normally take 5 mg prednisone daily, you might need to double or triple your dose during a fever or surgery to prevent adrenal crisis.
Frequently Asked Questions
What is ACTH stimulation testing, and why is it needed during steroid tapering?
The ACTH stimulation test measures your adrenal glands' ability to produce cortisol after long-term steroid use. During the test, synthetic ACTH is injected, and blood cortisol levels are checked at 0, 30, and 60 minutes. This test is critical because long-term steroids suppress your body's natural cortisol production. Without this test, doctors can't safely determine when to stop steroids completely. The 2024 Endocrine Society guidelines state that testing is critical for patients who've been on steroids for more than 3-4 weeks.
How long does adrenal recovery take after stopping steroids?
Recovery time varies based on treatment duration. For steroid use lasting 3-12 months, recovery typically takes 1 month per month of therapy. For example, a 6-month treatment might require 6 months of tapering. For therapy exceeding 12 months, recovery can take up to 9-12 months. The Adrenal Insufficiency Coalition's 2020 guideline notes that adrenal atrophy increases with longer steroid exposure, making gradual tapering essential to avoid permanent adrenal insufficiency.
What are the risks of skipping ACTH testing during steroid tapering?
Skipping ACTH testing significantly increases the risk of adrenal crisis-a life-threatening condition marked by severe fatigue, vomiting, low blood pressure, and shock. A 2023 study in the Journal of Clinical Endocrinology & Metabolism found that protocols using ACTH testing reduced adrenal crisis rates by 86% compared to symptom-based approaches alone. Without testing, doctors can't confirm if your adrenal glands have recovered, leading to dangerous gaps in care. For instance, 23% of patients in a 2023 survey reported ER visits due to testing delays, highlighting the critical need for this procedure.
Can I adjust my steroid dose on my own during tapering?
No. Adjusting steroid doses without medical supervision can lead to adrenal crisis or disease reactivation. The Endocrine Society's 2024 guideline emphasizes that 'the dosage started and the rate of taper are entirely dependent on the disease response.' For example, in Duchenne muscular dystrophy, abrupt changes can cause muscle function decline. Always follow your doctor's specific tapering schedule and consult them before any dose changes.
How do stress doses work during illness or surgery?
Stress doses are extra steroids given during physical stress like illness, surgery, or injury to prevent adrenal crisis. For example, if you normally take 5 mg prednisone daily, you might need to double or triple your dose during a fever or surgery. The PJ Nicholoff Protocol provides detailed stress dosing tables for different scenarios. The American Association of Clinical Endocrinology reports 92% compliance in academic centers but only 47% in community practices-underscoring the importance of patient education on this critical step.
Katharine Meiler
February 6, 2026 AT 02:30The ACTH stimulation test is critical for monitoring adrenal function during steroid tapering. Mayo Clinic data shows a significant reduction in adrenal crisis rates. However, access remains a challenge, especially in rural areas. Proper implementation requires coordination between endocrinologists and primary care.
Danielle Vila
February 7, 2026 AT 01:11Big Pharma is using ACTH testing to keep patients on steroids longer.
Joyce cuypers
February 7, 2026 AT 15:04This is so helpul! I learned a lot. Keep up the good work!
Carol Woulfe
February 8, 2026 AT 11:46The current guidelines are woefully inadequate. Only those with proper medical training should be allowed to interpret ACTH results. The general public is ill-equipped to understand this complex physiology.
Kieran Griffiths
February 10, 2026 AT 03:48Great post! The details on the PJ Nicholoff Protocol are spot on. Especially for Duchenne patients.
Lisa Scott
February 11, 2026 AT 16:38ACTH testing is a scam
Tehya Wilson
February 12, 2026 AT 01:35Testing unnecessary patients should be trusted to self manage this is bureaucratic nonsense
Brendan Ferguson
February 13, 2026 AT 19:59Many patients struggle with steroid tapering due to lack of access to endocrinologists.
The ACTH stimulation test is a critical tool for monitoring adrenal recovery, but rural areas face significant barriers.
Telehealth could bridge this gap, but there's a shortage of specialists willing to participate.
Additionally, primary care physicians often lack training in interpreting results.
A 2023 study found that 68% of primary care doctors felt unprepared to handle ACTH testing.
This highlights the need for better education and resource allocation.
Furthermore, insurance companies often don't cover the test, creating financial hurdles.
Patient advocacy groups are pushing for policy changes, but progress is slow.
In my own experience, I've seen patients delay tapering unnecessarily due to testing delays.
It's crucial to address these systemic issues to improve outcomes.
Collaboration between healthcare providers, policymakers, and patient advocates is essential.
We need standardized protocols for rural healthcare.
Also, integrating telemedicine with endocrinology consultations could make testing more accessible.
Training programs for primary care doctors would help them recognize when to refer.
Ultimately, the goal is to prevent adrenal crises through timely testing and proper care.
This requires systemic change, not just individual efforts.
We must prioritize patient safety over bureaucratic hurdles.
jan civil
February 15, 2026 AT 03:14The HPA axis details were very clear. Important to remember cortisol needs time to recover.
Gregory Rodriguez
February 16, 2026 AT 01:18Wow, finally someone who gets it. This is the most useful thing I've read all week. Not.
Johanna Pan
February 17, 2026 AT 05:03Very informative post! I learned so much. Though I think the guidelines could be more global. There's a typo: 'adrenel' instead of 'adrenal'.
Jenna Elliott
February 18, 2026 AT 21:03US should lead in this other countries dont know what theyre doing testing is key but theyre ignoring it
Elliot Alejo
February 20, 2026 AT 02:29Solid info. The table comparing guidelines is helpful. Should be mandatory for all doctors.