Medication-Assisted Treatment Explained
When talking about medication-assisted treatment, a coordinated approach that blends FDA‑approved medication with behavioral counseling to help people stop using opioids, alcohol, or nicotine. Also known as MAT, it aims to reduce cravings, prevent relapse, and improve overall health. Buprenorphine, a partial opioid agonist that eases withdrawal without producing the high of full agonists is often the first line for opioid dependence. Methadone, a long‑acting full agonist administered in certified clinics provides stable dosing for severe cases. Naltrexone, an opioid antagonist that blocks the effects of any opioid taken works well for those who have completed detox. Finally, behavioral counseling, structured therapy sessions that teach coping skills and address underlying triggers rounds out the program, making sure medication isn’t used in isolation.
Why blend meds with therapy? The science shows that medication alone lowers mortality but doesn’t fully address the psychological grip of addiction. Counseling adds a cognitive layer—patients learn how to handle stress, rebuild relationships, and set realistic goals. In practice, a typical MAT plan starts with an assessment, chooses the appropriate drug based on severity, and schedules weekly or monthly counseling. The dosage is adjusted until cravings subside, then the focus shifts to tapering or maintenance while therapy continues. This synergy creates a safety net: if cravings spike, the medication cushions the impact; if medication is missed, counseling offers an early warning system.
Key Benefits You’ll Notice Quickly
Clients on MAT report fewer withdrawal symptoms within the first week, more stable sleep, and a gradual return to daily routines. Hospital readmissions drop by about 50 % compared with detox‑only approaches, according to recent health‑system data. Moreover, people on buprenorphine or methadone are less likely to engage in risky behaviors like sharing needles, which cuts down on infections such as hepatitis C. Naltrexone, though not a pain reliever, blocks the euphoria from any opioid use, acting as a deterrent after detox. When combined with counseling, these medical gains translate into higher employment rates and stronger family ties within months.
Choosing the right medication isn’t a one‑size‑fits‑all decision. Buprenorphine suits patients who need flexibility—its ceiling effect reduces overdose risk, and it can be prescribed in office settings. Methadone is best for those with long histories of heavy use; its daily clinic visits enforce structure but require more commitment. Naltrexone fits individuals who have already achieved abstinence and want a non‑opioid safeguard. Each drug carries its own side‑effect profile—buprenorphine may cause mild constipation, methadone can lengthen QT intervals, and naltrexone might trigger liver enzyme changes. A qualified prescriber weighs these factors alongside personal health history.
Behavioral counseling comes in many flavors: cognitive‑behavioral therapy (CBT), motivational interviewing, and contingency management are the most common. CBT helps patients identify thought patterns that lead to use and replace them with healthier responses. Motivational interviewing taps into personal reasons for change, boosting commitment. Contingency management rewards drug‑free urine tests with vouchers or privileges, reinforcing positive behavior. Programs often blend all three, adjusting intensity based on progress. The goal isn’t just abstinence; it’s sustainable lifestyle change.
If you’re considering MAT, start by locating a certified provider—most states list them online, and many primary‑care doctors now hold waivers to prescribe buprenorphine. Bring a list of current medications, any liver or heart issues, and be ready to discuss your substance use openly. Expect an initial intake interview, a treatment agreement, and a baseline lab work panel. After the first dose, you’ll schedule follow‑up visits to monitor cravings, side effects, and mental‑health status. Remember, the process is iterative; dose tweaks and counseling adjustments are normal.
Below you’ll find a curated set of articles that dive deeper into each medication, compare alternatives, and explore counseling techniques. Whether you’re a patient, a family member, or a health professional, these pieces give you the facts you need to make informed decisions about medication-assisted treatment and its role in lasting recovery.
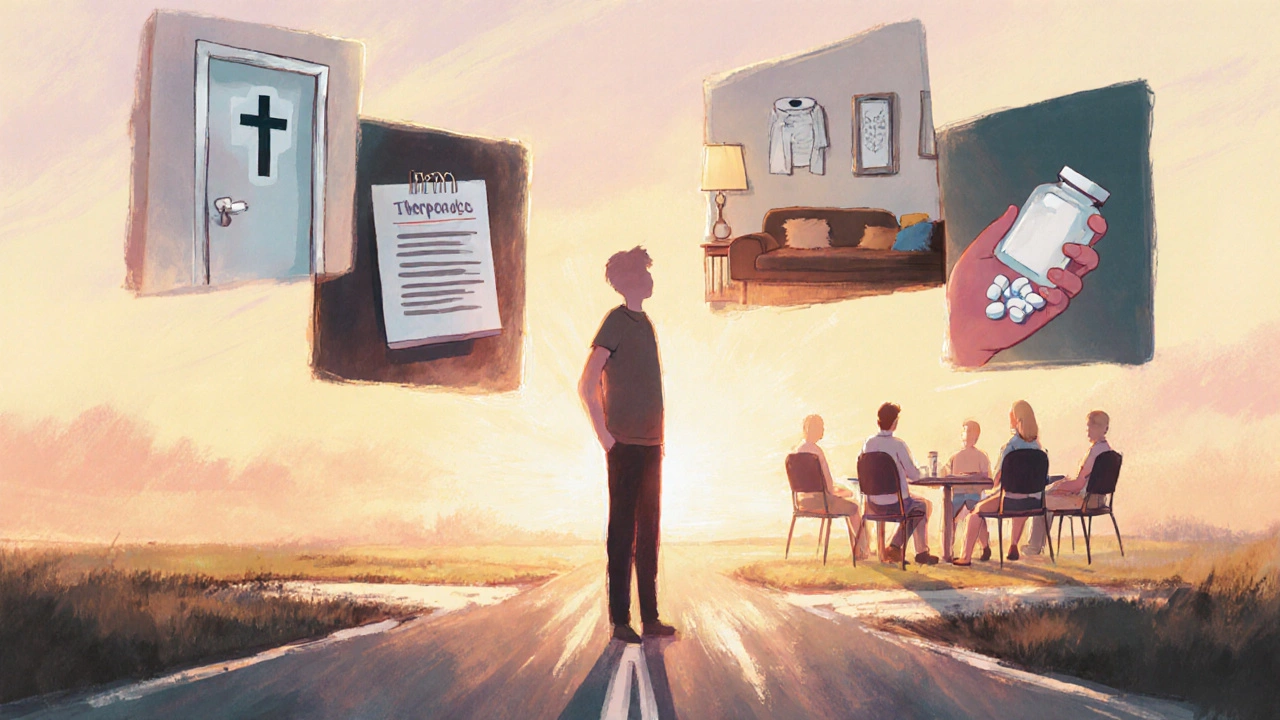
Alcoholism Treatment Options: Inpatient, Meds, Therapy & Support
Explore the full range of alcoholism treatments-from detox and inpatient rehab to medication, therapy, and support groups-plus how to choose the right plan for lasting sobriety.