Alcoholism Treatment Options: Inpatient, Meds, Therapy & Support
 Oct, 8 2025
Oct, 8 2025
Alcoholism Treatment Pathway Planner
Based on your answers, this tool recommends a personalized treatment path. Here's what each option involves:
- Detox - Removes alcohol from the body under medical supervision
- Inpatient Rehab - Intensive 28-90 day residential treatment
- Outpatient Therapy - Flexible weekly counseling sessions
- MAT - Medication-assisted treatment to manage cravings
- Support Groups - Peer-led meetings for accountability
- Dual Diagnosis - Integrated treatment for mental health and alcohol issues
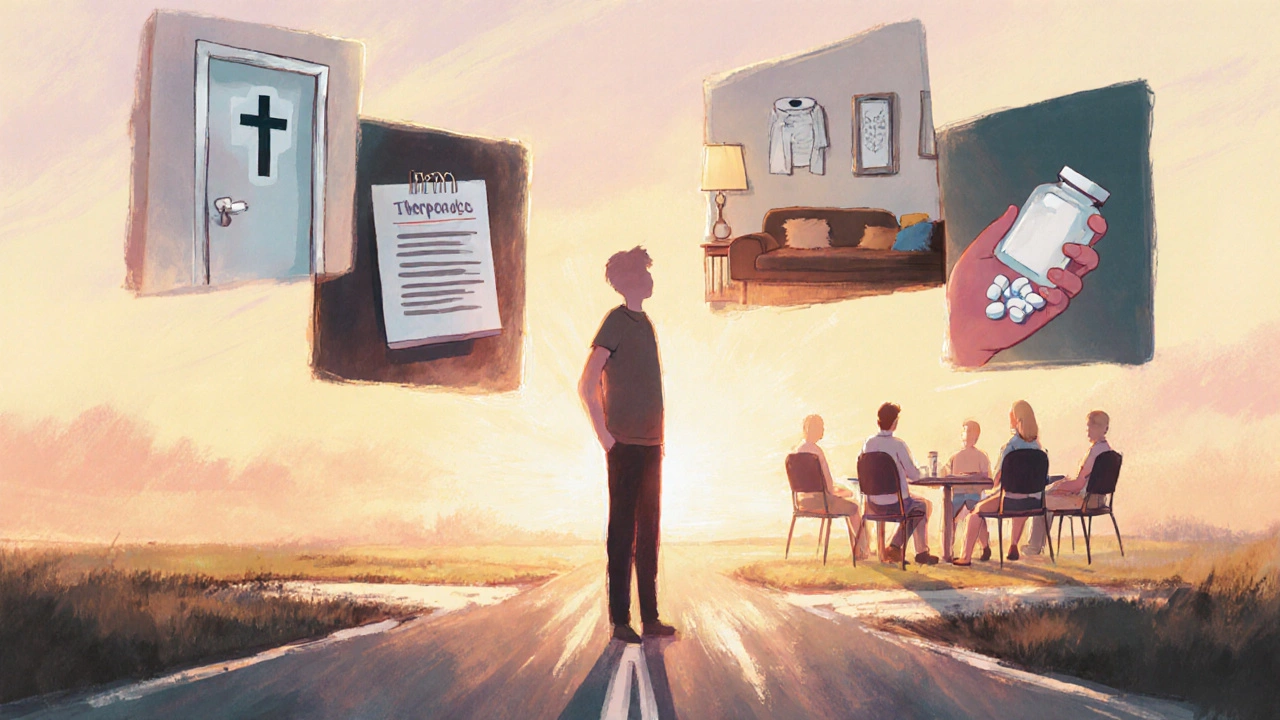
When alcohol dependence takes over, figuring out the right way to break free feels overwhelming. Luckily, there isn’t a one‑size‑fits‑all answer-there’s a whole menu of proven treatments that fit different lifestyles, severity levels, and personal preferences. Below you’ll find a straight‑talk guide to the major options, how they work, and where to start.
Alcoholism is a chronic disease characterized by an inability to control drinking despite negative consequences. It affects roughly 5% of adults worldwide and often co‑exists with mental‑health issues, making a tailored treatment plan essential.Why One Approach Rarely Works Alone
Recovery is usually a mix of medical, behavioral, and social support. Think of it like fixing a car: you might need a new engine (detox), upgraded tires (therapy), and regular oil changes (support groups). Skipping any piece can leave you stuck.
1. Detoxification - The First Step
Detox isn’t a cure, but it clears the alcohol from the system and manages withdrawal symptoms that can be life‑threatening. It’s typically done in a hospital or specialized detox center under medical supervision.
- Duration: 3-7 days (sometimes longer for heavy users)
- Medications used: benzodiazepines, anticonvulsants, thiamine
- Cost: varies by facility; public hospitals may be subsidized
After detox, the real work begins-choosing a longer‑term program.
2. Inpatient Rehabilitation
Inpatient rehab is a live‑in treatment setting where patients stay 24/7 for a structured program that blends medical care, therapy, and peer support. It’s best for people with severe dependence, co‑occurring disorders, or unstable home environments.
- Typical stay: 28‑90 days
- Key features: daily counseling, group therapy, recreational activities
- Success metric: 6‑month abstinence rates of 40‑60% in well‑run programs
While costs can be high-often $10,000‑$30,000 per month-many insurers cover part of the expense, and government subsidies exist in several regions.

3. Outpatient Counseling & Therapy
Outpatient programs let you live at home while attending scheduled therapy sessions. They’re ideal for those with work, family, or milder dependence.
Cognitive Behavioral Therapy (CBT) helps patients identify triggers, challenge cravings, and develop coping skills. Motivational Interviewing (MI) focuses on boosting intrinsic motivation to change drinking behavior.- Frequency: 2-5 sessions per week
- Duration: 12‑24 weeks
- Cost: $100‑$200 per session (often covered by insurance)
Combining CBT and MI yields higher abstinence rates than either alone, according to a 2023 multicenter trial.
4. Medication‑Assisted Treatment (MAT)
Medication‑assisted treatment uses FDA‑approved drugs to reduce cravings, block alcohol’s effects, or stabilize mood. The three most common meds are:
- Naltrexone - blocks opioid receptors, reducing the rewarding feeling of alcohol.
- Acamprosate - restores the balance of brain chemicals disrupted by chronic drinking.
- Disulfiram - causes an acute reaction (flushed skin, nausea) if alcohol is consumed.
MAT works best when paired with counseling. In a 2022 meta‑analysis, combined MAT and therapy produced a 30% higher abstinence rate than therapy alone.
5. Support Groups
Peer‑led meetings provide accountability, shared experience, and hope. The most recognized models are:
- 12‑Step Programs such as Alcoholics Anonymous (AA) - emphasize spiritual growth and a sponsor relationship.
- SMART Recovery - uses CBT principles, focuses on self‑empowerment.
- Secular Organizations for Sobriety (SOS) - offers a non‑religious framework.
Attendance is free, and many people report sustained sobriety after regular participation.
6. Integrated Dual‑Diagnosis Programs
If you’re dealing with depression, anxiety, or PTSD alongside alcoholism, look for programs that treat both simultaneously. Integrated care reduces relapse risk by 25% compared with treating each condition separately.

Choosing the Right Path
Here’s a quick decision flow you can run through yourself:
- Assess severity: severe (withdrawal seizures, multiple failed attempts) → consider detox + inpatient rehab.
- Check support network: weak family or workplace support → inpatient or intensive outpatient.
- Identify co‑occurring issues: mental‑health diagnoses → dual‑diagnosis program.
- Preference for meds? → discuss MAT with a physician.
- Need flexibility? → outpatient counseling + support groups.
Remember, you can start with one option and add others later. Many people begin with detox, then move to outpatient CBT while attending AA.
Practical Steps to Get Started Today
- Talk to your primary care doctor or a local addiction specialist about detox options.
- Ask about insurance coverage for inpatient vs. outpatient care.
- Research nearby rehab centers; read patient reviews and accreditation status.
- If medication sounds right, request a prescription for naltrexone or acamprosate and set up a follow‑up counseling appointment.
- Find a support group that fits your schedule-most cities have multiple meetings per week.
- Set short‑term goals (e.g., attend three therapy sessions, avoid drinking for 48hours) and track progress.
Small, consistent actions create momentum toward lasting sobriety.
Key Takeaways
- Detox is the medically supervised start; it doesn’t replace ongoing treatment.
- Inpatient rehab offers intensive, round‑the‑clock support for high‑risk individuals.
- Outpatient therapy (CBT, MI) works well for moderate cases and maintains daily life responsibilities.
- Medication‑assisted treatment can curb cravings and improve success when paired with counseling.
- Support groups provide peer accountability and are free to join.
- Dual‑diagnosis programs address co‑occurring mental‑health disorders, boosting overall outcomes.
| Option | Setting | Typical Duration | Medication Use | Best For |
|---|---|---|---|---|
| Detoxification | Hospital or specialized center | 3-7 days | Yes (sedatives, thiamine) | Severe physical dependence, safety first |
| Inpatient Rehabilitation | Live‑in facility | 28-90 days | Optional (often includes MAT) | High‑risk drinkers, unstable home life |
| Outpatient Counseling | Clinic or telehealth | 12-24 weeks | Optional (MAT) | Moderate dependence, work/family commitments |
| Medication‑Assisted Treatment | Prescribed by doctor, taken at home | Ongoing, often 6+ months | Yes (naltrexone, acamprosate, disulfiram) | Craving control, relapse prevention |
| Support Groups | Community meetings (in‑person/online) | Ongoing | No | Long‑term accountability, peer support |
| Dual‑Diagnosis Programs | Integrated medical/behavioral setting | Varies (often 3-6 months) | Often includes MAT & psychiatric meds | Co‑occurring mental‑health disorders |
Frequently Asked Questions
Is detox enough to become sober?
Detox only removes alcohol from the body and manages immediate withdrawal. Without follow‑up therapy, medication, or support, relapse rates are high-often above 70% within three months.
Can I take naltrexone if I’m pregnant?
Naltrexone is not recommended during pregnancy because safety data are limited. Pregnant individuals should discuss alternative plans with their obstetrician.
Do support groups cost anything?
Most community‑run groups like AA and SMART Recovery are free. Some specialized or therapist‑led groups may charge a modest fee.
How long does inpatient rehab typically last?
Programs usually range from 28 days to 90 days, with longer stays reserved for complex cases or co‑occurring disorders.
Can I combine medication‑assisted treatment with therapy?
Yes, combining MAT (like naltrexone) with CBT or MI dramatically improves abstinence rates and is considered best practice.
Ryan Hlavaty
October 8, 2025 AT 12:56Honestly, if you’re not willing to admit that alcoholism is a disease and not just a lack of willpower, you’re doing yourself and everyone around you a massive disservice. The world is full of people who think they can quit whenever they feel like it, and they end up dragging families into ruin. It’s not just about a night out; it’s about the slow, relentless erosion of health, finances, and relationships. People need to get serious, seek professional help, and stop romanticizing “just one drink”. Anything less is practically a moral failing, and that’s the reality we need to face.
Chris Faber
October 8, 2025 AT 13:21I get that the whole thing can feel overwhelming but there are actually a lot of options that fit different lifestyles. Whether you need a short detox or a longer rehab stay, you can find something that works for you without turning your whole life upside down.
aura green
October 8, 2025 AT 13:46Look, the first thing you have to realize is that recovery isn’t a one‑size‑fits‑all checklist that you can just tick off because you feel like it, it’s a marathon, not a sprint, and you’ll probably stumble many times before you finally get a rhythm that feels sustainable, which is why the combination of medication‑assisted treatment and therapy is so crucial because it tackles both the physiological cravings and the psychological triggers, and let’s be honest, most people who try to quit cold turkey end up either relapsing or spending a fortune on emergency room visits, which is why a structured outpatient program can give you that needed accountability while still letting you keep a job, and if you have co‑occurring mental health issues like depression or anxiety, a dual‑diagnosis program can actually double your chances of staying sober, which is corroborated by multiple studies, and the beauty of support groups is that they’re free and you get to hear stories from people who’ve been there, which is incredibly grounding, and don’t forget that the right medication, like naltrexone or acamprosate, can blunt the pleasure you get from alcohol, making it easier to stick to your goals, and if you’re worried about side effects, just talk to a doctor who can tailor the dosage, and remember that the journey is personal – what works for your cousin might not work for you, so stay flexible, be kind to yourself, and keep trying new combinations until you find the sweet spot, because quitting drinking is tough, but you don’t have to do it alone 😅
Edward Morrow
October 8, 2025 AT 14:03Pull yourself together.
Shayne Tremblay
October 8, 2025 AT 14:20Hey there! 🌟 If you’ve been thinking about taking the first step, remember that every small victory counts – even a single day without a drink is a win. Keep setting realistic goals, celebrate your progress, and lean on supportive friends or groups when the cravings hit. You’ve got this, and the road to recovery is totally worth the effort!
Stephen Richter
October 8, 2025 AT 14:36It is noteworthy that the original post provides a comprehensive overview of treatment modalities. However, the omission of insurance navigation strategies may hinder accessibility for many individuals. Prospective patients should be directed toward resources that facilitate coverage inquiries and financial assistance programs. Moreover, a clearer delineation between detox and long‑term therapy phases would enhance the guide's practicality. Finally, inclusion of post‑rehab relapse prevention techniques would further strengthen the utility of the article.
Musa Bwanali
October 8, 2025 AT 14:53Totally agree with the need for a balanced approach – you can’t just throw medication at the problem without building coping skills, and you definitely don’t want to rely solely on talk therapy if cravings are gnawing at you. A solid mix of both, plus a supportive community, makes the biggest difference.
Allison Sprague
October 8, 2025 AT 15:10While the article is informative, it could benefit from stricter adherence to medical terminology. Phrases like “feel better” are vague; instead, specify measurable outcomes such as reductions in GGT levels or improvements in PHQ‑9 scores. This precision will aid clinicians and patients alike.
leo calzoni
October 8, 2025 AT 15:26Honestly, the guide sounds like it was written by someone who has never actually helped a patient. It’s all fluff and no concrete steps. If you’re serious about recovery, you need a plan that tells you exactly what to do, not just vague suggestions.
KaCee Weber
October 8, 2025 AT 15:43Great article! 😊 I especially love the section about combining medication with therapy – it’s such a game‑changer. Also, the reminder that support groups are free is super helpful for anyone on a tight budget. Keep up the good work! 🙌
jess belcher
October 8, 2025 AT 16:00It would be beneficial to add a brief summary at the end for quick reference. A concise table highlighting key points could serve readers who need a fast overview.
Sriram K
October 8, 2025 AT 16:16From a clinical perspective, it’s important to stress that medication adherence is critical. Many patients discontinue meds prematurely, which undermines effectiveness. Regular follow‑ups and patient education can mitigate this issue.
Deborah Summerfelt
October 8, 2025 AT 16:33One could argue that labeling all these treatments as “proven” is a stretch, given the variability in study designs and populations. Nonetheless, offering options is better than a one‑size‑fit‑all approach.
Maud Pauwels
October 8, 2025 AT 16:50While I respect the comprehensive nature of the piece, I would caution readers to verify the credibility of any program before committing.
Scott Richardson
October 8, 2025 AT 17:06Let’s not forget that many of these programs are pricey. If you can’t afford them, the article should suggest low‑cost alternatives.
Laurie Princiotto
October 8, 2025 AT 17:23…or you could just keep drinking and ignore all this nonsense 😒
Justin Atkins
October 8, 2025 AT 17:40In summation, a multi‑modal treatment paradigm, integrating pharmacotherapy, psychotherapy, and peer support, represents the current gold standard for alcohol use disorder management. Such an approach is substantiated by a robust body of literature demonstrating superior outcomes relative to monotherapy.
June Wx
October 8, 2025 AT 17:56Honestly, the whole “you gotta go to rehab” narrative is overblown. Lots of folks just need a solid therapist and maybe a med – no need for a fancy brick‑and‑mortar center.
kristina b
October 8, 2025 AT 18:13It is incumbent upon us, as a society, to recognize that the journey toward sobriety is not merely a personal odyssey but a collective moral imperative; the structures we erect – be they clinical institutions or community support webs – must therefore be forged with compassion, scientific rigor, and an unwavering commitment to the dignity of each individual who seeks redemption from the shackles of dependence. In this light, the integration of evidence‑based pharmacological agents with psychotherapeutic modalities emerges not as a convenience but as a requisite, a symphony of interventions wherein each note – the neurochemical stabilization provided by naltrexone or acamprosate, the cognitive restructuring facilitated by CBT, the shared narratives within AA meetings – coalesces to produce a harmonious path toward lasting recovery. Let us, therefore, champion policies that expand access, dismantle stigma, and nurture the communal bonds that render the solitary pursuit of sobriety a shared triumph.