Warfarin and NSAIDs: Why Combining Them Raises Bleeding Risk
 Nov, 23 2025
Nov, 23 2025
Warfarin & NSAID Risk Calculator
Calculate Your Bleeding Risk
See how much your bleeding risk increases with specific NSAIDs while taking warfarin
Combining warfarin and NSAIDs isn't just a bad idea-it’s dangerous. If you're taking warfarin for atrial fibrillation, a mechanical heart valve, or deep vein thrombosis, and you reach for ibuprofen or naproxen for a headache or sore knee, you're putting yourself at serious risk. This isn't speculation. It's backed by decades of research, hospital data, and clinical guidelines that all say the same thing: warfarin and NSAIDs together can trigger life-threatening bleeding.
How Warfarin Works (And Why It’s Already a Tightrope Walk)
Warfarin doesn’t thin your blood like water. It slows down your body’s ability to make clotting factors. Specifically, it blocks vitamin K, which your liver needs to produce factors II, VII, IX, and X. Without those, clots form slower. That’s good if you’re at risk of a stroke or clot blocking an artery. But if you get cut, bruise, or even develop a small tear in your stomach lining, your body can’t seal it quickly enough.
Your doctor checks your INR (International Normalized Ratio) regularly to make sure your blood clots at the right speed. An INR of 2.0-3.0 is typical for most people on warfarin. Go above 4.0? Your bleeding risk jumps. Go below 1.5? Your clot risk rises. It’s a narrow window-and NSAIDs can easily push you out of it.
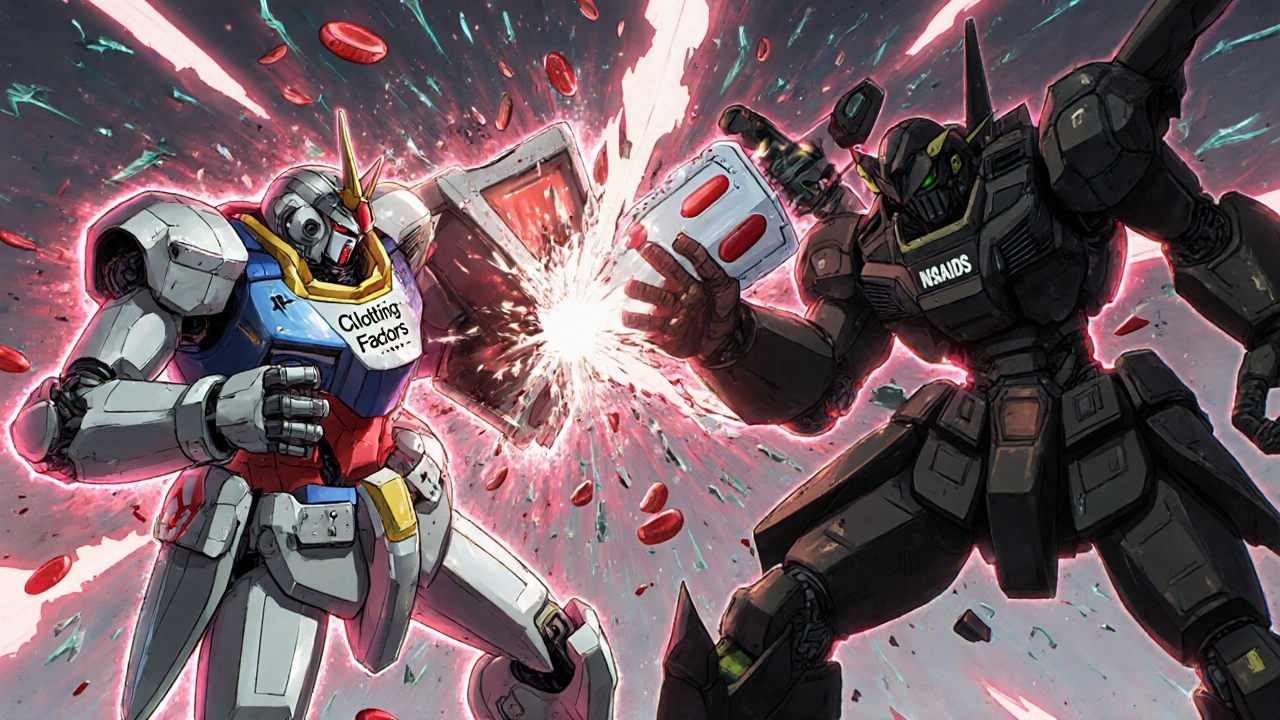
How NSAIDs Make Things Worse
NSAIDs-like ibuprofen, naproxen, diclofenac, and even low-dose aspirin-don’t just reduce pain and inflammation. They also interfere with platelets, the tiny blood cells that plug leaks in damaged blood vessels. They do this by blocking COX-1, an enzyme that helps make thromboxane A2, a chemical that tells platelets to stick together.
Think of it like this: warfarin makes your blood slower to clot. NSAIDs make your platelets less able to form the first seal. Together, they’re like turning off both the glue and the tape when you’re trying to fix a leaky pipe.
And it gets worse. NSAIDs also damage the stomach lining. They reduce prostaglandins, which normally protect your stomach from acid. That’s why people on NSAIDs get ulcers. When you add warfarin into the mix, those tiny ulcers or erosions don’t heal. They bleed. And because warfarin keeps the bleeding from stopping, it doesn’t just cause discomfort-it can lead to massive internal bleeding.
The Numbers Don’t Lie: How Much Higher Is the Risk?
Studies show the risk isn’t just slightly higher-it’s dramatically higher.
- People taking both warfarin and an NSAID are more than twice as likely to have a major bleed compared to those on warfarin alone.
- For gastrointestinal bleeding, the risk jumps by 2 times.
- Brain bleeds (intracranial hemorrhage) become 3.2 times more likely.
- Naproxen? It raises bleeding risk by 4.1 times.
- Diclofenac? 3.3 times.
- Ibuprofen? Still 1.8 times higher-even though it’s often seen as "safer."
And it’s not just about the stomach. Bleeding can happen in the lungs, kidneys, urinary tract, or even under the skin. One study found that NSAID users on warfarin had nearly three times the risk of developing anemia from bleeding-because their bodies couldn’t replace the lost blood fast enough.
Who’s at Highest Risk?
Not everyone on warfarin who takes an NSAID will bleed. But some people are far more vulnerable:
- Those on high-dose warfarin (>40 mg per week): Their INR is already harder to control. Adding an NSAID pushes it out of range faster.
- People with low baseline INR: If your INR is usually on the lower end (say, 2.0), your body has less "buffer" before bleeding starts.
- Those taking other medications: Antibiotics, antifungals, or even some herbal supplements (like garlic or ginkgo) can also affect warfarin. Add an NSAID? Risk multiplies.
- People using meloxicam: One study found meloxicam was independently linked to INR spikes-more than other NSAIDs.
Age matters too. People over 65 are more likely to have stomach issues, weaker blood vessels, and slower drug clearance. That’s why guidelines are even stricter for older adults.
What About Newer Blood Thinners? Are They Safer?
Many people switch from warfarin to DOACs like apixaban, rivaroxaban, or dabigatran because they don’t need regular INR checks. But here’s the catch: NSAIDs still raise bleeding risk with these drugs too.
A 2018 study found that while dabigatran didn’t interact with NSAIDs *more* than warfarin, the absolute risk of bleeding-especially in the gut-was still significantly higher when NSAIDs were added. And here’s something surprising: with DOACs, 60% of major bleeds happened outside the gut. That means even if you don’t have stomach pain, you could still be bleeding internally.
Bottom line: NO blood thinner is safe with NSAIDs. The risk is real, regardless of whether you’re on warfarin or a newer drug.
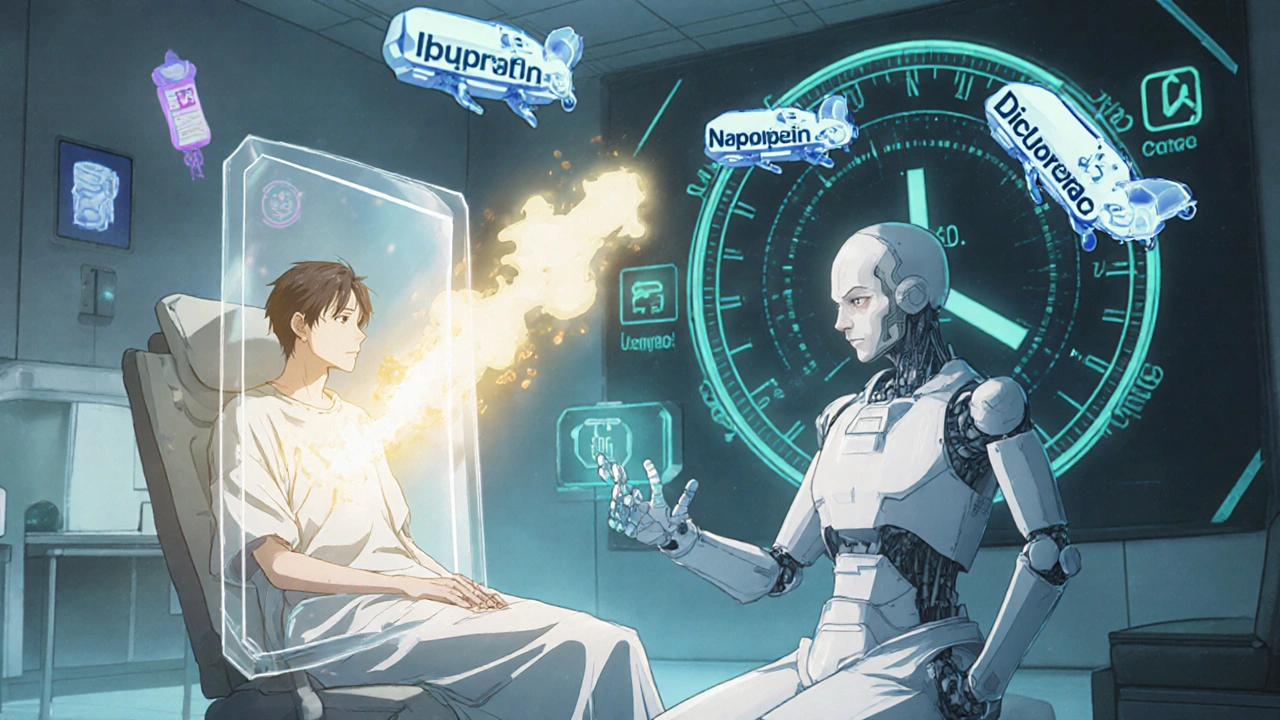
What Should You Do Instead?
You don’t have to suffer through pain just because you’re on warfarin. There are safer options:
- Acetaminophen (paracetamol): Up to 3,000 mg per day is generally safe for most people on warfarin. It doesn’t affect platelets or the stomach lining. It’s your first-line pain reliever.
- Topical pain relievers: Gels or patches with diclofenac or menthol applied directly to the skin (like Voltaren Gel) deliver pain relief without raising your blood’s bleeding risk.
- Physical therapy, heat, or ice: For joint or muscle pain, these non-drug options can be just as effective-and zero risk.
- Low-dose aspirin for heart protection: If your doctor prescribed low-dose aspirin for heart disease, don’t stop it. But tell them you’re on warfarin. They’ll need to monitor you closely.
If you absolutely must take an NSAID-for example, after surgery or for severe arthritis-your doctor should:
- Use the lowest effective dose for the shortest time possible.
- Prescribe a proton pump inhibitor (PPI) like pantoprazole 40 mg daily to protect your stomach.
- Check your INR within 3-5 days after starting the NSAID, then weekly until stable.
- Avoid naproxen and diclofenac if possible. Ibuprofen is less risky-but still risky.
What to Watch For: Signs of Bleeding
If you’re on warfarin and take an NSAID-even once-know the warning signs:
- Bleeding gums when brushing teeth
- Nosebleeds that won’t stop
- Unexplained bruising, especially large or dark patches
- Red or black, tarry stools
- Bloody or pink urine
- Severe headache, dizziness, vision changes (possible brain bleed)
- Weakness, fatigue, or shortness of breath (signs of anemia from blood loss)
If you notice any of these, stop the NSAID and call your doctor immediately. Don’t wait. Don’t assume it’s "just a bruise."
Why This Still Happens-And How to Prevent It
Despite all the evidence, a 2022 study found that nearly 29% of warfarin users got an NSAID prescription within a year. That’s not just a mistake-it’s a system failure. Pharmacists don’t always flag it. Doctors forget. Patients don’t know.
You have to be your own advocate. Always tell every healthcare provider you’re on warfarin. Keep a list of all your meds-including over-the-counter pills and supplements. Ask: "Is this safe with warfarin?" If they say "probably," push back. The data is clear: it’s not "probably" unsafe. It’s definitely unsafe.
There’s no magic pill that makes NSAIDs safe with warfarin. The only reliable way to avoid bleeding is to avoid the combination. Your body doesn’t need extra painkillers to function. It needs safety.
Can I take ibuprofen with warfarin if I only use it once in a while?
Even a single dose of ibuprofen can raise your INR and increase bleeding risk, especially if you’re on a higher warfarin dose or have other risk factors. It’s not worth the gamble. Use acetaminophen instead. If you’re in severe pain and think you need ibuprofen, talk to your doctor first-don’t self-medicate.
Is naproxen worse than ibuprofen with warfarin?
Yes. Naproxen increases bleeding risk by 4.1 times compared to warfarin alone-nearly double the risk of ibuprofen (1.8 times). It also stays in your system longer, meaning its effect on platelets lasts longer. Avoid naproxen entirely if you’re on warfarin.
What about topical NSAIDs like Voltaren Gel?
Topical NSAIDs are much safer because very little enters your bloodstream. Studies show they don’t significantly affect INR or bleeding risk. If you have joint pain, this is a good option. Just avoid applying it to broken skin or large areas for long periods.
Should I stop my NSAID before a blood test?
If you’ve taken an NSAID in the past 72 hours, tell your lab or doctor. It can affect your INR reading. If you’re scheduled for a routine INR check, avoid NSAIDs for at least 3 days before unless your doctor says otherwise. Consistency matters more than one-off use.
Can I take aspirin with warfarin?
Low-dose aspirin (81 mg) is sometimes used alongside warfarin for heart protection-but only under strict medical supervision. It increases bleeding risk significantly. Never combine them without your doctor’s approval. If you’re on both, you’ll need more frequent INR checks and likely a stomach-protecting medication.
Final Takeaway: Don’t Guess. Ask.
Warfarin is a powerful tool. But it’s not a casual medication. NSAIDs are common. But they’re not harmless when paired with it. The science is clear: together, they create a perfect storm for bleeding. You don’t need to live in pain. You just need to choose safer alternatives and speak up when something doesn’t feel right. Your next INR test could save your life-but only if you avoid the drugs that push it too high.
David Cunningham
November 24, 2025 AT 19:02Been on warfarin for 5 years and never touched NSAIDs. Acetaminophen and ice packs saved my knees. Simple stuff.
Ravi Kumar Gupta
November 25, 2025 AT 18:56Bro in India we take ibuprofen with everything. My uncle took warfarin and naproxen for 3 years and lived to 82. You Westerners overthink everything. Body knows what to do.
Rahul Kanakarajan
November 26, 2025 AT 18:38So let me get this straight. You're telling me that people who've been taking ibuprofen for decades with warfarin are just lucky and didn't bleed out? This is fearmongering dressed as science. If it was that dangerous, why isn't the FDA banning NSAIDs outright? Because it's not. It's about profit margins and liability. People die from acetaminophen overdoses too. Pick your poison.
New Yorkers
November 27, 2025 AT 19:39Warfarin is the original biohack. It's not a drug, it's a meditation on mortality. NSAIDs? They're the ego's desperate plea for comfort in a world that refuses to stop hurting. You can't out-ibuprofen your existential vulnerability. The body bleeds because it remembers. And so should you.
Daniel Jean-Baptiste
November 29, 2025 AT 02:28Just had my INR checked last week and my doc said no NSAIDs. I asked about topical diclofenac and she said that's fine. I've been using Voltaren Gel on my elbow for two months and no issues. Just gotta be smart about it. Also, paracetamol is my best friend now. No drama, no bleeding, just relief.
Jessica Correa
November 30, 2025 AT 23:09My mom took naproxen for arthritis and warfarin for AFib. She had a GI bleed at 78. They didn't know why until they saw the meds. She's fine now but it scared the hell out of us. Don't be that person who thinks 'once won't hurt'. It only takes once.
manish chaturvedi
December 2, 2025 AT 16:37In India, we often use ginger tea, turmeric paste, and warm oil massage for joint pain. These are safe, traditional, and effective. Why reach for a chemical when nature offers solutions? Warfarin requires respect. NSAIDs show disrespect. Choose wisely.
Miruna Alexandru
December 3, 2025 AT 03:44Interesting how the article cites studies showing 4.1x risk with naproxen but fails to mention the absolute risk increase. If baseline risk is 1.2% per year, 4.1x is still only 4.9%. The fear is amplified by relative risk. Also, the study on meloxicam was observational with confounding variables. Please stop using 'the numbers don't lie' as a rhetorical weapon when the numbers are being selectively interpreted.
Nikhil Chaurasia
December 3, 2025 AT 12:14My cousin took ibuprofen once for a migraine while on warfarin. He didn't bleed. He didn't even feel anything. He's alive. Maybe the risk is overstated? I'm not saying to take it, but not everyone bleeds. Maybe we need better personalization instead of blanket warnings?
luke young
December 4, 2025 AT 11:36Hey, I get what you're saying. But I think the article makes a good point - even if you're fine once, you don't know who’s next. I had a friend who thought the same thing. One time. One naproxen. One internal bleed. He’s okay now, but spent 10 days in ICU. Not worth it. Stick with Tylenol. Your body will thank you.
Shawn Daughhetee
December 5, 2025 AT 07:05My grandma's on warfarin and she uses those menthol patches for her back. No problems. I told her to always check with her pharmacist before trying anything new. She says she does. Honestly, if you're careful and communicate, you can manage this. Don't panic, just be smart.
ann smith
December 6, 2025 AT 22:15Thank you for this. I was so scared after my INR spiked last month and I realized I'd taken Advil for my headache. I switched to Tylenol and started using heat wraps. I feel so much better now. I'm not perfect but I'm trying. 💪❤️
Julie Pulvino
December 7, 2025 AT 10:20I love how this post ends with 'don't guess, ask.' That's the whole thing right there. My pharmacist caught me trying to refill naproxen last year. She didn't yell. She just said 'let's find you something safer.' We switched me to acetaminophen and a physical therapist. Best decision I ever made. You're not alone in this.