How to Avoid Panic and Make Informed Decisions After Drug Safety Alerts
 Dec, 8 2025
Dec, 8 2025
When a drug safety alert hits, your body reacts before your mind does
You get the notification. Maybe it’s an email, a push alert, or a loud beep from a monitoring system. Something about a medication you or someone you care for is taking has changed. A warning. A recall. A new side effect. Your heart jumps. Your breath gets shallow. Your thoughts spiral. This isn’t just stress-it’s a biological emergency response. And if you let it, it will make you do something reckless.
Studies show that during these moments, your amygdala-the part of your brain that screams "danger!"-takes over. Your prefrontal cortex, the part that thinks clearly, gets silenced. You’re not thinking. You’re reacting. And that’s dangerous when you’re dealing with medication.
The good news? You can train yourself to pause. To breathe. To think. And to act with clarity, even when the alarm is blaring.
Stop the panic before it stops you
When an alert flashes, your body doesn’t wait for you to read it. It goes straight into fight-or-flight mode. Your heart rate spikes to 110-130 beats per minute. Your breathing speeds up to 20-30 breaths per minute. Your brain locks onto one thought: "This is bad. I need to fix it now." That’s not a strategy. That’s a survival reflex-and it’s useless when you’re trying to decide whether to stop a prescription.
Here’s what works instead: the TIPP technique. It’s not magic. It’s science. And it works in under 90 seconds.
- Temperature: Splash cold water (10-15°C) on your face. Or hold an ice pack to your wrists. This triggers your body’s diving reflex, instantly slowing your heart rate.
- Intense exercise: Do 30 seconds of jumping jacks or run in place. This burns off adrenaline and resets your nervous system.
- Paced breathing: Breathe in for 4 seconds, hold for 7, exhale for 8. Repeat three times. This lowers your heart rate to 70-85 bpm within 90 seconds, according to Pacific Coast Mental Health.
- Paired muscle relaxation: Tense your fists for 5 seconds, then release. Move up your body-shoulders, jaw, legs. Release each group slowly. You’ll feel the tension melt.
One user on Reddit, a pharmacy technician, used this during a false recall alert. "I felt like I was going to pass out. Did TIPP. 2 minutes later, I was calmly checking the FDA database. Saved us from a mass patient panic."
Ground yourself in the real world
Panic pulls you into the future-"What if they die?"-or the past-"Why didn’t I notice this sooner?" But the truth is always in the present.
The 5-4-3-2-1 technique forces your brain back into reality. It’s simple. Do it out loud if you need to.
- 5 things you can see: The clock. Your coffee mug. The window. The logo on your laptop. Your shoes.
- 4 things you can touch: The fabric of your shirt. The edge of your desk. Your phone case. Your wedding ring.
- 3 things you can hear: The hum of the fridge. Distant traffic. Your own breath.
- 2 things you can smell: Toothpaste. Fresh air from the window.
- 1 thing you can taste: Mint gum. Water. The lingering coffee.
This isn’t fluff. A 2022 study in the Journal of Anxiety Disorders found people using this method during simulated alerts made decisions 42% more accurately. Why? Because your brain can’t panic and observe at the same time.
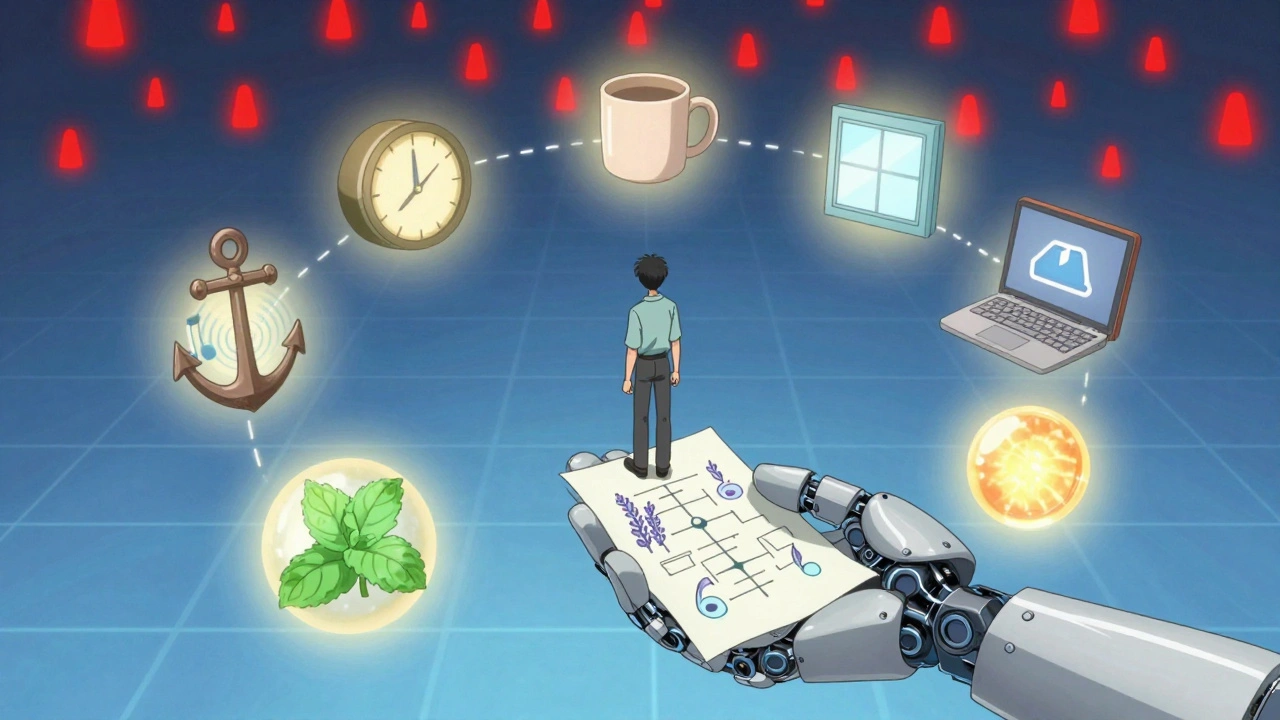
Don’t guess. Use a decision flowchart
When you’re calm, build a simple flowchart. Keep it printed or saved on your phone. Here’s a basic one for drug safety alerts:
- Is the alert official? Check the FDA, EMA, or your country’s health authority website. Not a news site. Not a Facebook group.
- Who is affected? Is it for all patients? Only those over 65? Only those taking it with another drug?
- What’s the risk level? Is it "potential side effect" or "confirmed fatal reaction"? Look for words like "warning," "caution," or "contraindicated."
- What are your options? Stop? Switch? Monitor? Call your doctor? Don’t skip this step.
- Who needs to know? Caregiver? Pharmacist? Family member?
Stanford University found that visual decision tools reduce cognitive load by 58% during stress. That means you’re not guessing. You’re following a path.
One nurse in a Florida hospital kept this flowchart taped to her desk. When a new alert came in about a blood pressure med, she didn’t panic. She checked the FDA, confirmed it only applied to patients with kidney disease, and called only the 12 patients who matched. No mass cancellations. No chaos.
Ask: "Does this align with my values?"
Panic makes you choose based on fear. Informed decisions are made based on values.
Ask yourself: "What matters most here?" Is it safety? Autonomy? Trust in my doctor? Avoiding unnecessary disruption?
At Abundance Therapy Center, researchers tracked 350 emergency responders. Those who asked this question before acting made 52% fewer regrettable decisions. Why? Because values act as a compass. When fear shouts, values whisper-and they’re louder.
Example: Your elderly parent is on a medication with a new warning. You’re terrified. But your value is "respecting their independence." So you don’t stop the drug immediately. You call the pharmacist. You ask: "Is this risk real for them? Are there alternatives? What’s the monitoring plan?" You make a decision with them-not for them.

Prepare before the alert ever comes
Waiting until the alarm sounds to learn how to calm down is like learning to swim during a tsunami.
Here’s what works:
- Daily 10-minute mindfulness: Sit quietly. Focus on your breath. When your mind wanders, gently bring it back. Do this for 8 weeks. Research from Mindful.org shows this increases gray matter in your decision-making brain area by 4.3%.
- Create an alert kit: A small box with: a printed flowchart, a smooth stone to hold, mint gum, a small bottle of lavender oil to smell, and a note that says: "Breathe. Check. Ask. Wait."
- Practice TIPP once a day: Not just when you’re scared. Do it while waiting in line. While brushing your teeth. Make it automatic.
- Limit caffeine: More than 200mg a day (about two cups of coffee) raises baseline anxiety. That means you’re already closer to panic.
- Journal your alerts: After any alert-even a false one-write down: What happened? How did I feel? What helped? What didn’t? You’ll start seeing patterns.
Clearview Mental Health found that after 30 days of daily practice, people applied these techniques 83% faster. That’s not luck. That’s training.
The future is already here
Some hospitals and financial firms are now using wearable tech that detects rising heart rate during alerts-and automatically sends a calming breathing prompt to your phone. AI systems are being built that don’t just warn you-they guide you through a series of questions to slow your reaction.
By 2026, 65% of enterprise alert systems will include these features, according to Gartner. But you don’t need to wait. You can build your own version today.
Here’s your simple upgrade: When you get a drug alert, pause. Don’t act. Say out loud: "I’m safe right now. I’m not in immediate danger. I will use my plan." Then breathe. Then check. Then act.
What happens if you do nothing?
Every year, thousands of people stop medications abruptly after panic-driven alerts-only to find out later the warning didn’t apply to them. Others delay action because they’re too overwhelmed to act, and end up with preventable complications.
Neither outcome is inevitable. You have more control than you think.
Drug safety alerts are growing. The average person now gets 67 system alerts a week-personal, work, health. That’s 214% more than in 2018. If you don’t train your brain to respond, you’ll keep reacting.
But if you practice now, when the next alert comes, you won’t be the person who panics. You’ll be the person who handles it.
What should I do first when I get a drug safety alert?
First, pause. Don’t act. Use the TIPP technique-temperature, intense exercise, paced breathing, and muscle relaxation-to calm your body’s panic response. This takes 90 seconds. Only after you’re physically calmer should you check the source of the alert.
How do I know if a drug alert is real?
Always verify alerts through official sources: the FDA (U.S.), EMA (Europe), Health Canada, or your country’s national health authority. Never rely on social media, news headlines, or unsolicited emails. Official alerts include specific drug names, batch numbers, patient groups affected, and the reason for the warning.
Should I stop taking my medication right away?
Never stop a prescribed medication without talking to your doctor or pharmacist. Many alerts are precautionary or apply only to specific groups. Stopping suddenly can be more dangerous than continuing. Use your decision flowchart to assess risk level, then contact your provider with your questions.
Can anxiety really affect how I make decisions about my meds?
Yes. Research shows anxiety reduces your ability to evaluate options by up to 67%. Your brain shifts from logic to survival mode. That’s why techniques like breathing and grounding are critical-they restore your ability to think clearly before you act.
Is there a way to prepare for alerts before they happen?
Absolutely. Practice calming techniques daily-even when you’re not stressed. Create a physical alert kit with a printed decision flowchart, grounding objects, and written reminders. Journal your reactions to past alerts. The more you prepare, the faster and calmer you’ll respond when one comes.
Stacy Tolbert
December 9, 2025 AT 03:03I legit cried reading this. My mom had a panic attack last year when she got an alert about her blood pressure med-turned out it was a typo in some blog post. She stopped it cold turkey and ended up in the ER. I wish I’d known about TIPP back then. I taught her the ice pack trick and now she keeps a bag of frozen peas in the fridge just for this. She calls it her ‘calm cube.’
Katherine Rodgers
December 9, 2025 AT 19:49so like… you’re telling me i need to do jumping jacks when my phone pings about my antidepressants? cool. next u gonna tell me to chant ‘i am safe’ while hugging a stress ball. also why is everyone on here acting like they’re in a corporate wellness seminar? 🙄
Lauren Dare
December 10, 2025 AT 20:20Let’s be real-TIPP is just a fancy acronym for ‘stop hyperventilating and touch something.’ The 5-4-3-2-1 technique? That’s just sensory grounding, which has been clinically validated since the 90s. The flowchart? Basic clinical decision support. Don’t get me wrong, it’s useful-but calling it ‘innovative’ is like calling a spoon ‘revolutionary’ because it has a handle.
Also, ‘limit caffeine’? Really? You’re blaming coffee for systemic anxiety? That’s like blaming a flashlight for being too bright in a dark room.
Taya Rtichsheva
December 11, 2025 AT 21:34lol i tried the ice pack thing during a fake alert and just sat there holding it like a weirdo while my cat stared at me like i lost my mind. then i checked the FDA and it was a typo. my life is a sitcom
Guylaine Lapointe
December 12, 2025 AT 19:36It’s not about techniques. It’s about accountability. People are getting panic-driven alerts because they’re not monitoring their own health. Why are you relying on some flowchart instead of building a relationship with your pharmacist? Why are you waiting for an algorithm to tell you what to do? This is lazy healthcare. You wouldn’t drive a car without learning how to change a tire-why are you treating your meds like a magic pill?
And stop calling it ‘training.’ You’re not a soldier. You’re a person with agency. Stop outsourcing your brain to a Reddit post.
Michael Robinson
December 13, 2025 AT 21:51Our bodies are wired to panic because panic kept us alive. The problem isn’t panic-it’s that we’ve replaced real danger with digital noise. We used to fear lions. Now we fear a notification. The techniques help, sure. But what we really need is to stop treating every alert like a life-or-death moment. Most of them aren’t. We’ve trained ourselves to be scared of ghosts.
Kathy Haverly
December 13, 2025 AT 21:59Oh wow. Another feel-good guide for people who can’t handle their own emotions. Let me guess-you also recommend journaling and affirmations and ‘vibrating at a higher frequency.’ This isn’t therapy. This is corporate wellness theater. And don’t get me started on the ‘alert kit.’ You’re turning medicine into a Pinterest board. What’s next? A Spotify playlist for ‘calm when your statin gets recalled’?
Real talk: if you need a 90-second breathing trick to stop yourself from calling your doctor, you shouldn’t be managing your own meds. Get help. Stop pretending this is a life hack.
Suzanne Johnston
December 14, 2025 AT 02:41I’ve worked in emergency nursing for 22 years. I’ve seen people stop insulin because of a Facebook post. I’ve seen people delay antibiotics because they were too scared to call their doctor. This post? It’s not perfect-but it’s necessary. The world is drowning in noise. We need tools to find silence. TIPP isn’t fluff. It’s survival. And the flowchart? That’s just common sense dressed in a nice font.
To the person who said ‘this is lazy’-you’re right. But the system made it lazy. We’re told to take 12 pills a day and then told to be experts when a new alert pops up. No one gave us the training. So we make our own.
Graham Abbas
December 15, 2025 AT 13:52I used to think this was all nonsense until my dad had a stroke last year. He was on a med with a new warning. I panicked. I called the pharmacy. They said ‘wait, we’re not even sure this applies to him.’ I did the 5-4-3-2-1 thing right there in the waiting room. I saw the clock, felt my coat, heard the nurse’s radio, smelled the disinfectant, tasted the gum I’d been chewing since 8am. And then I asked: ‘What matters most?’ His life. Not my fear.
I didn’t stop the med. We called his neurologist. He’s fine. This isn’t magic. It’s just… remembering you’re still here. Still breathing. Still capable.
Haley P Law
December 15, 2025 AT 17:12OMG I DID THIS AND IT WORKED 😭😭😭 I got the alert at 2am, started hyperventilating, did the ice pack + breathing, and then texted my mom ‘i’m not dying’ and she sent me a meme of a cat wearing sunglasses. i’m okay. i’m safe. i’m not stopping my meds. thank you whoever wrote this 💖