Osteoarthritis vs Rheumatoid Arthritis: Understanding Key Differences
 Feb, 4 2026
Feb, 4 2026
Over 32 million American adults live with osteoarthritis - that’s ten times more than rheumatoid arthritis. Yet most people can’t tell the difference between these two common joint conditions. Why does it matter? Because treating them wrong can lead to serious consequences. Let’s break down the real differences between OsteoarthritisA degenerative joint disease caused by mechanical wear and tear on joints, leading to cartilage breakdown and bone-on-bone contact. and Rheumatoid ArthritisAn autoimmune disorder where the immune system attacks healthy joint tissue, causing systemic inflammation and damage..
How Osteoarthritis Actually Works
Osteoarthritis (OA) is pure mechanical damage. Think of it like the cushion between your bones wearing out from years of use. Cartilage - the smooth, rubbery tissue that protects your joints - gradually breaks down. Without it, bones rub against each other. This causes pain, swelling, and stiffness. OA most often hits weight-bearing joints like knees and hips, but it also commonly affects hand joints, especially the ones closest to your fingertips. Unlike other arthritis types, OA isn’t caused by your immune system. It’s simply the result of aging, past injuries, or excess body weight putting too much stress on joints.
One telltale sign of OA is how symptoms change with activity. Pain usually gets worse when you move the joint and improves with rest. Morning stiffness typically lasts less than 30 minutes. If you have OA in your hands, you might notice bony bumps near your fingertips - called Heberden’s nodes. X-rays will show joint space narrowing and bone spurs. Weight loss is a game-changer here: losing just 5 kilograms reduces knee OA pain by about 50%, according to ArthritisCARE’s 2023 data.
What Makes Rheumatoid Arthritis Different
Rheumatoid arthritis (RA) is your immune system going rogue. Instead of protecting you, it attacks the lining of your joints (synovium), causing inflammation that damages cartilage and bone. This isn’t just about joints - RA is a systemic disease that can affect your lungs, heart, eyes, and even skin. Unlike OA, RA often starts in smaller joints like wrists and fingers, but it always affects both sides of the body symmetrically. If your left wrist hurts, your right will too.
RA symptoms develop faster than OA - often within weeks or months. Morning stiffness lasts longer than an hour, and you’ll likely feel tired, have low fevers, or lose weight unexpectedly. Blood tests are crucial for diagnosis: Rheumatoid factorAn antibody commonly found in the blood of people with rheumatoid arthritis. (RF) and Anti-CCP antibodiesA more specific blood test for rheumatoid arthritis that helps confirm diagnosis. (anti-cyclic citrullinated peptide) are key markers. Without treatment, RA can destroy joints in just months. Doctors now recommend starting DMARDsDisease-modifying antirheumatic drugs that slow down joint damage in rheumatoid arthritis. within the first 3-6 months of symptoms for the best outcomes.
Side-by-Side Comparison of Symptoms
| Aspect | Osteoarthritis | Rheumatoid Arthritis |
|---|---|---|
| Primary Cause | Joint wear and tear | Autoimmune attack on joint lining |
| Onset Speed | Gradual (years) | Rapid (weeks to months) |
| Morning Stiffness | Less than 30 minutes | Over 60 minutes |
| Joint Pattern | Asymmetrical (one side affected) | Symmetrical (both sides affected) |
| Systemic Symptoms | None | Fatigue, fever, weight loss |
| Diagnostic Test | X-rays showing bone spurs | Blood tests for RF and anti-CCP |
Other Arthritis Types You Should Know
While OA and RA make up most arthritis cases, other types exist. Psoriatic arthritisA form of inflammatory arthritis linked to psoriasis skin disease. often comes with scaly skin patches and affects nails. GoutA type of arthritis caused by uric acid crystal buildup in joints. hits suddenly, usually in the big toe, with intense pain. Juvenile Idiopathic ArthritisChronic arthritis affecting children under 16 years old. is the most common type in kids. Each has unique triggers and treatments, but OA and RA remain the most diagnosed.
Why Getting the Right Diagnosis Matters
Mixing up OA and RA can be dangerous. OA treatment focuses on pain relief and joint protection - things like NSAIDs, physical therapy, and weight management. But RA needs aggressive immune-suppressing drugs like DMARDs to stop joint damage. If RA is mistaken for OA, critical treatment gets delayed. By the time damage is visible on X-rays, it’s often too late to prevent permanent disability. Experts agree: early intervention for RA within the first six months changes long-term outcomes dramatically.
Treatment Realities for Each Condition
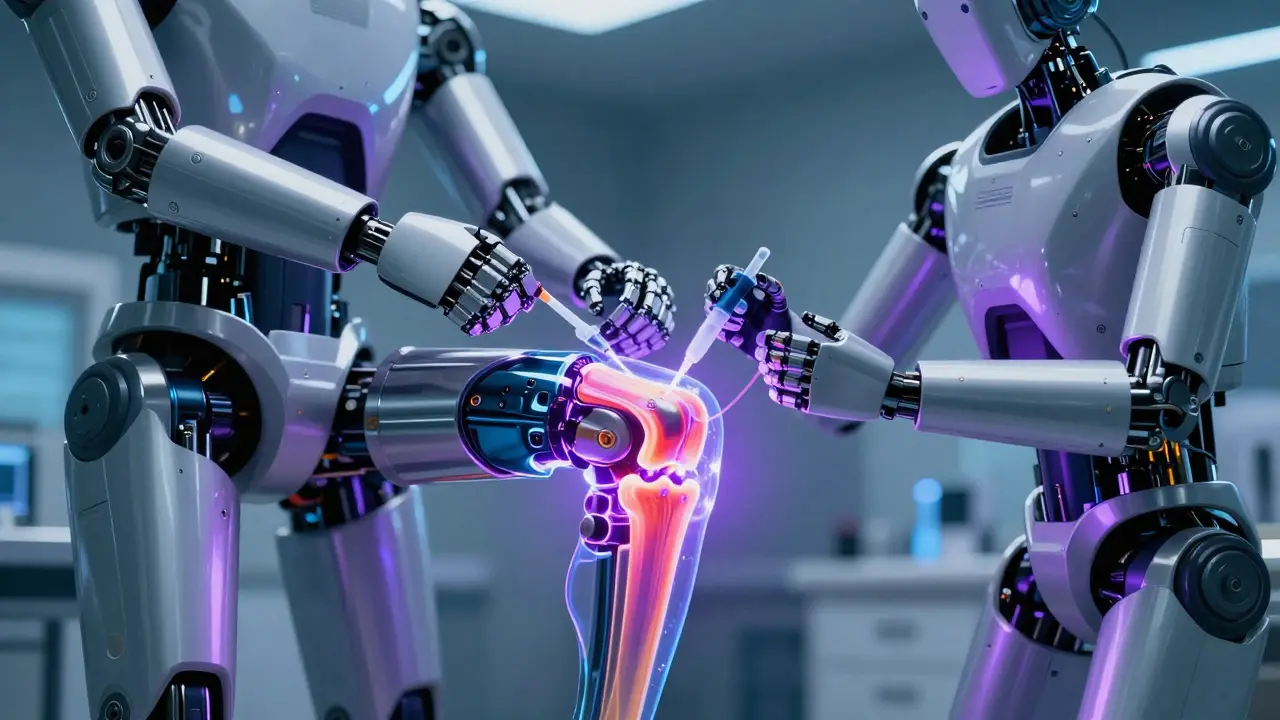
For OA, lifestyle changes are foundational. Losing weight, low-impact exercise like swimming, and using joint supports can slow progression. Pain management usually starts with acetaminophen or NSAIDs like ibuprofen. When joints are severely damaged, Joint replacement surgerySurgical procedure to replace damaged joints with artificial implants. is common - about 90% of all joint replacements in the U.S. are for OA.
RA treatment is more complex. First-line therapy is methotrexate, a DMARD that suppresses the immune system. If that fails, biologic drugs like TNF inhibitors are used. These can cost $20,000-$50,000 yearly but are life-changing for many. Newer options like JAK inhibitors (e.g., tofacitinib) offer alternatives, though they come with increased infection risks. Smoking worsens RA significantly - current smokers have two to three times higher risk of developing it.
Can you have both osteoarthritis and rheumatoid arthritis?
Yes, though it’s rare. OA is from mechanical wear, while RA is autoimmune. Having one doesn’t cause the other, but they can coexist. For example, someone with RA might develop OA in the same joint due to years of inflammation. Doctors need to check for both when symptoms don’t match typical patterns.
How do doctors tell them apart?
Blood tests are key for RA - rheumatoid factor and anti-CCP antibodies are positive in most cases. OA diagnosis relies on X-rays showing joint space narrowing and bone spurs. Symptom patterns also help: OA pain worsens with activity and improves with rest, while RA causes prolonged morning stiffness and symmetrical joint involvement. A rheumatologist can usually spot the difference with these clues.
Is there a cure for either condition?
No cure exists for either OA or RA. However, RA can go into remission with proper treatment - about 30-50% of patients achieve this with early DMARD use. OA management focuses on slowing progression through weight control, exercise, and pain relief. While joint replacement surgery can restore function in severe OA, it doesn’t stop the underlying wear-and-tear process.
What are the biggest risk factors?
For OA: obesity (BMI over 30 increases knee OA risk 4.5-fold), joint injuries, and aging. For RA: smoking (doubles risk), genetic markers like HLA-DRB1, and family history. Interestingly, while OA is more common in women over 50, RA affects women three times more often than men across all ages.
Can lifestyle changes help?
Absolutely. Weight loss is the most effective OA intervention - every kilogram lost reduces knee joint stress by four kilograms. For RA, quitting smoking is critical. Low-impact exercises like walking or tai chi improve mobility for both conditions. Diet also plays a role: omega-3 fatty acids (from fish oil) reduce inflammation in RA, while avoiding processed sugars helps control OA flare-ups.
Albert Lua
February 6, 2026 AT 07:10As a cultural ambassador, I've seen how different countries handle arthritis. In Japan, they use traditional medicine like acupuncture and herbal remedies which complement Western treatments. It's fascinating how global perspectives can enhance patient care. We should learn from each other.
Dina Santorelli
February 7, 2026 AT 07:00Environmental toxins and GMOs are the real causes of arthritis. The data is outdated and biased. I've been dealing with this for years and it's all a scam. Big pharma is in on it. This is why people don't trust medical advice anymore.
Carl Crista
February 8, 2026 AT 18:57OA and RA are the same thing caused by vaccines and the government is hiding the cure.
Nancy Maneely
February 8, 2026 AT 20:005G is causing arthritis. The US is the only country that knows the truth. Big pharma is hiding it. I'm so mad! 😤
Diana Phe
February 9, 2026 AT 01:13US is the best. Other countries are clueless. Big pharma is in cahoots with the government. They don't want you to know the real cause. It's all about control. Wake up people!
Cole Streeper
February 10, 2026 AT 23:23Big pharma is pushing fake arthritis treatments to keep people dependent. They know OA and RA are the same but split them to sell more drugs. USA is the only country with real solutions, but they're suppressing the truth. I've seen studies showing the government is in on it.
divya shetty
February 11, 2026 AT 08:56As a healthcare professional from India, I must correct this article. The statistics are incorrect. In our country, the prevalence is different. Also, the treatment options are not as described. This is very irresponsible.
Katharine Meiler
February 11, 2026 AT 18:34Biomarkers like anti-CCP are more specific than RF, but newer markers like citrullinated vimentin are emerging. It's important to consider these in diagnosis to avoid misclassification.
Phoebe Norman
February 13, 2026 AT 16:25RA is autoimmune synovitis leading to systemic inflammation but OA is mechanical degeneration however the article fails to mention the role of cytokines like IL-6 and TNF-alpha in RA progression which is critical for understanding treatment options
Samantha Beye
February 14, 2026 AT 05:34Starting DMARDs early for RA is crucial. Many people don't realize this. I've seen patients do so much better when they catch it early.
Rene Krikhaar
February 14, 2026 AT 18:15I've treated many arthritis patients and the key is personalized care. OA needs weight management while RA needs aggressive treatment. But doctors should listen to patients more. We need better communication
Matthew Morales
February 16, 2026 AT 16:33I had no idea about the differences. Eating more omega-3s helps RA. Typos: 'causes' instead of 'cause' but still useful!
Jennifer Aronson
February 18, 2026 AT 00:05As someone who's worked in international healthcare for over 15 years, I've seen firsthand how arthritis management differs across cultures. In Japan, traditional medicine like acupuncture and herbal remedies are commonly integrated with Western treatments, leading to better patient outcomes. In India, Ayurvedic practices such as turmeric and yoga are used alongside conventional drugs. In Scandinavian countries, there's a strong focus on physical therapy and lifestyle modifications from the earliest stages. Meanwhile, in parts of Africa, access to medications is limited, so communities rely on natural remedies and community support systems. This diversity in approaches shows that there's no one-size-fits-all solution for arthritis. It's crucial for healthcare providers to be aware of these cultural differences to tailor treatment plans effectively. For example, a patient from a culture that values herbal medicine might respond better to a combined approach rather than solely relying on pharmaceuticals. Additionally, understanding a patient's cultural background can improve adherence to treatment plans and overall satisfaction with care. I've also noticed that in some regions, the stigma around chronic conditions like arthritis leads to delayed diagnosis and treatment, which worsens outcomes. Education and community outreach programs can play a significant role in reducing this stigma. Furthermore, collaboration between Western medicine and traditional healers can lead to innovative treatments that address both physical and emotional aspects of the disease. It's important for medical professionals to approach these topics with an open mind and respect for diverse healing traditions. Ultimately, the goal should be to provide holistic care that respects the patient's cultural context while leveraging the best of modern medicine. This integrated approach not only improves patient outcomes but also fosters greater trust between healthcare providers and the communities they serve.