Medications with a Narrow Therapeutic Index: Why Expiration Dates Matter More Than You Think
 Dec, 24 2025
Dec, 24 2025
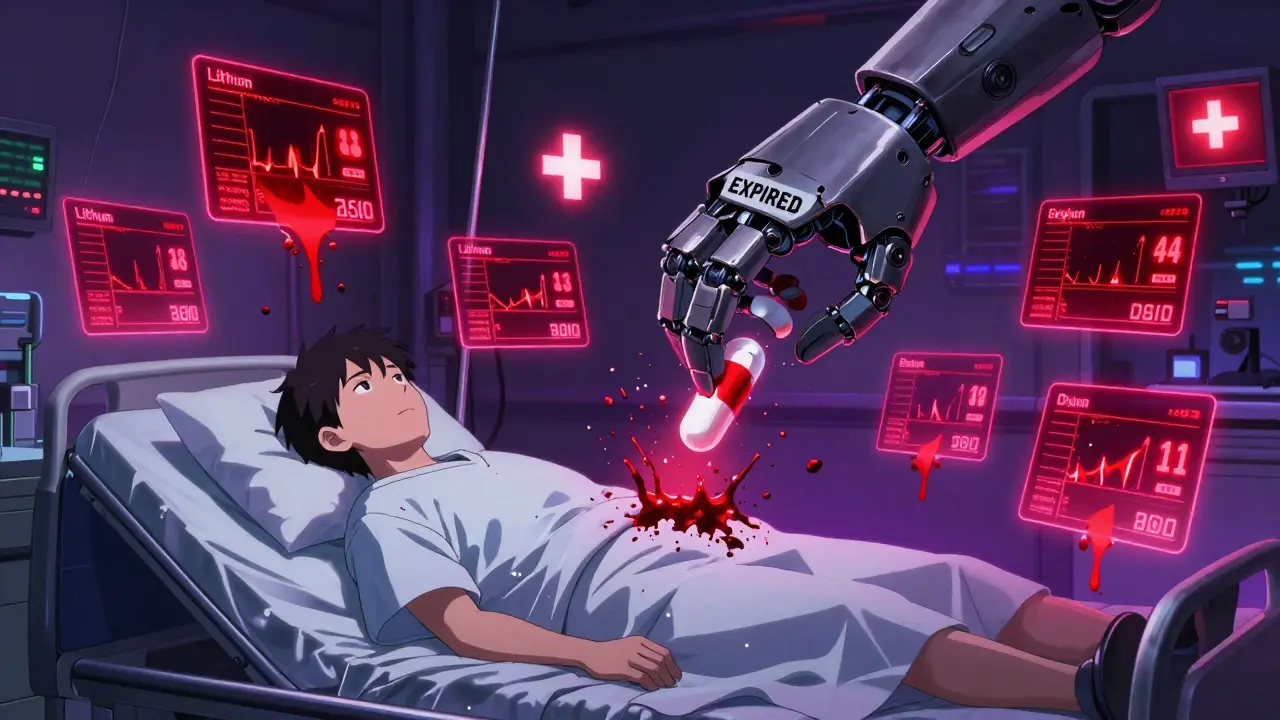
When you take a pill, you assume it does what it’s supposed to do. But for some medications, even a tiny change in strength can be dangerous-sometimes deadly. These are called narrow therapeutic index (NTI) drugs. They don’t play nice with variations. A little too much? You could bleed, have a seizure, or go into heart failure. A little too little? You could get a blood clot, have a seizure, or reject a transplanted organ. And if that pill is past its expiration date? The risk goes up-not because the drug turns toxic, but because it might not work at all.
What Exactly Is a Narrow Therapeutic Index?
Think of a therapeutic index as the gap between the dose that helps and the dose that hurts. For most medicines, that gap is wide. You can miss a dose, take it a little late, or even grab a different brand, and you’ll still be okay. Not so with NTI drugs. The difference between the right amount and the dangerous amount is razor-thin-often less than a twofold margin. That means if your blood level of the drug drops by 10% or rises by 10%, you’re no longer in the safe zone.
The U.S. Food and Drug Administration (FDA) defines NTI drugs as those where small changes in concentration can cause serious harm: hospitalization, disability, or death. This isn’t theoretical. It’s backed by decades of clinical data. Drugs like warfarin, lithium, digoxin, phenytoin, and levothyroxine fall into this category. For example, digoxin’s therapeutic range is 0.5 to 0.9 nanograms per milliliter. Toxicity starts above 1.2. That’s just a 33% increase from the top of the safe range to the point where your heart could start beating irregularly-or stop.
Why Expiration Dates Are Critical for NTI Drugs
Every medication has an expiration date. That’s not a marketing gimmick. It’s the last day the manufacturer guarantees the drug will be at least 90% potent and completely safe under proper storage conditions. For most drugs, losing 5-10% potency over time doesn’t matter much. But for NTI drugs, even a 5% drop can push you out of the therapeutic window.
Take warfarin. It’s used to prevent clots in people with artificial heart valves or atrial fibrillation. The target INR (a blood test that measures clotting time) is 2.0 to 3.0. If your INR drops below 2.0, you’re at risk of a stroke. Above 4.0, you risk major bleeding. A 10% loss in warfarin potency from an expired pill could lower your INR by 0.5 to 1.0 units-enough to slip you out of safety. That’s not speculation. Studies show exactly this happens.
And it’s not just about losing strength. Some drugs break down into harmful byproducts. Tetracycline is a classic example-expired, it can damage the kidneys. While tetracycline isn’t an NTI drug, the principle applies: degradation isn’t always harmless. For NTI drugs, we don’t have full data on every degradation product, but we know the margin for error is so small that any change must be treated as a threat.
How Much Can NTI Drugs Really Degrade After Expiration?
You might have heard that most medications stay effective for years past their expiration date. That’s true for many-especially if stored in cool, dry places. The FDA’s 1985 study found that 90% of drugs retained potency for at least five years beyond their label date. But here’s the catch: that study didn’t include NTI drugs. And it wasn’t measuring clinical outcomes. It was measuring chemical stability in a lab.
For NTI drugs, the standard 80-125% bioequivalence range used for generics doesn’t apply. The FDA requires a tighter 90-111% range for drugs like levothyroxine, carbamazepine, and phenytoin. That means even a 10% drop in potency would put the drug outside the acceptable range. If an expired NTI drug degrades by 5%, that’s 50% of the allowed variation gone. You’re already in uncharted territory.
And here’s what’s worse: NTI drugs often have unpredictable absorption. Phenytoin, for example, can be absorbed differently depending on food, stomach pH, or even the brand you’re using. If that same drug is also degraded, you’re stacking two unknowns on top of each other. No doctor can safely adjust a dose without knowing exactly what’s in the pill.
Real-World Risks: What Happens When People Use Expired NTI Drugs?
There aren’t many published case reports of people getting hurt from expired NTI drugs-partly because it’s hard to prove. But we know what happens when the dose is off.
Lithium, used for bipolar disorder, has a therapeutic range of 0.6 to 1.0 mmol/L. Toxicity starts around 1.5. A 30% drop in potency might make someone feel fine-until they start having tremors, confusion, or seizures. A 20% increase? They could end up in the ICU with kidney failure.
One study in the Journal of Clinical Pharmacy and Therapeutics found that drug-related problems with NTI medications were five times more likely to cause serious harm than with other drugs. Another study showed that 67% of pharmacists treat warfarin with extreme caution when switching brands. Imagine how much more cautious they should be when the pill is old.
Patients on immunosuppressants like cyclosporine or tacrolimus after organ transplants are especially vulnerable. A slight drop in drug levels can trigger organ rejection. A slight rise can cause kidney damage or nerve problems. These patients are monitored closely with blood tests. But if their medication is expired, those tests become meaningless. The doctor thinks the dose is right. The blood level looks normal. But the drug in the bottle isn’t what it used to be.
What Should You Do If You Have an Expired NTI Drug?
Don’t guess. Don’t risk it. Don’t take it.
If you find an expired NTI medication in your cabinet, the safest move is to dispose of it properly and get a new prescription. Pharmacies in Australia and the U.S. offer take-back programs for expired or unwanted medications. If you’re on a fixed income and worried about cost, talk to your doctor. Many manufacturers offer patient assistance programs. Generic versions of NTI drugs are available, but even generics must meet the tighter 90-111% standard. That doesn’t mean they’re interchangeable without monitoring-but they’re safer than expired stock.
Never refill an NTI drug without checking the expiration date. If your pharmacy gives you a bottle labeled “expires 12/2023” and you’re still taking it in 2025, ask why. If they say, “It’s probably fine,” walk out and go elsewhere. A good pharmacist will tell you: “For this medicine, we don’t take chances.”

How Doctors and Pharmacists Handle NTI Drugs
Healthcare providers know the stakes. The Institute for Safe Medication Practices classifies NTI drugs as “high-alert medications.” That means double-checks, independent verification, and clear labeling. Many hospitals require two nurses to verify doses of digoxin or warfarin before giving them.
Pharmacists are trained to flag NTI drugs in their systems. They won’t just hand you a bottle. They’ll ask: “Are you switching brands?” “Is this a refill?” “Has this been stored in a hot bathroom?”
Therapeutic drug monitoring (TDM) is standard for these drugs. Blood tests for lithium, phenytoin, or vancomycin aren’t optional-they’re routine. But TDM only works if the drug in your body is the same as the one on the label. If it’s degraded, the test gives you false confidence.
What’s Being Done to Improve Safety?
Regulators are slowly catching up. The FDA now requires stricter bioequivalence testing for four key NTI drugs: levothyroxine, phenytoin, carbamazepine, and tacrolimus. That’s a step forward. But there’s still no official guidance on expiration dates for these drugs.
Some manufacturers are going further. About 78% of major pharmaceutical companies now run extended stability testing on NTI drugs-beyond the labeled expiration date-to understand how they degrade. But that data isn’t public. Patients don’t get to see it.
Professional groups like the American Pharmacists Association are pushing for special labeling on NTI drugs: “Do not use after expiration. Store in original container at room temperature. Keep away from heat and moisture.” Simple. Clear. Life-saving.
Bottom Line: Don’t Take Chances With NTI Drugs
NTI drugs aren’t like painkillers or antacids. They’re precision tools. A small change in dose can change your life-or end it. Expiration dates exist for a reason. For these medications, that reason is survival.
If you take warfarin, lithium, digoxin, phenytoin, levothyroxine, or any other NTI drug:
- Check the expiration date every time you refill.
- Never use a pill past its expiration date, even if it looks fine.
- Store your meds in a cool, dry place-not the bathroom or a sunny windowsill.
- Ask your pharmacist: “Is this the same brand I was on before?”
- If you miss a dose or feel off, don’t assume it’s your body. Ask if your medication could be the issue.
There’s no such thing as “just one more pill” with an NTI drug. One pill can be the difference between walking out of the hospital-and not.
What does it mean if a drug has a narrow therapeutic index?
A narrow therapeutic index means the difference between the dose that works and the dose that causes harm is very small. Even a slight change in blood levels-like from a degraded or expired pill-can lead to serious side effects, including hospitalization or death. Examples include warfarin, lithium, and digoxin.
Can expired NTI drugs become toxic?
Some expired drugs can break down into harmful substances, like tetracycline. While most NTI drugs don’t turn toxic, they often lose potency. For drugs like warfarin or lithium, even a 5-10% drop in strength can push you below the therapeutic level, causing clots, seizures, or organ rejection. The danger isn’t always toxicity-it’s underdosing.
How long after expiration are NTI drugs still safe to use?
There’s no safe window. While some medications retain potency for years, NTI drugs are too sensitive to risk it. Even if a pill looks fine, its strength may have dropped enough to be ineffective. The FDA doesn’t test NTI drugs for long-term stability, so there’s no data to support using them past the labeled date. Always replace them.
Are generic NTI drugs safe to use?
Yes-but only if they meet stricter bioequivalence standards. The FDA requires generics of NTI drugs like levothyroxine and phenytoin to be within 90-111% of the brand-name version, compared to 80-125% for most drugs. Even then, switching brands can affect blood levels. Always monitor closely and don’t switch without your doctor’s approval.
Should I throw away expired NTI medications?
Yes. Do not keep or use them. Many pharmacies and hospitals have take-back programs for expired drugs. If you can’t find one, mix the pills with coffee grounds or cat litter, seal them in a container, and throw them in the trash. Never flush them unless instructed. But above all-don’t take them.
Oluwatosin Ayodele
December 26, 2025 AT 03:53Let me tell you something you won't hear from Big Pharma: expiration dates are a scam. I've been taking my warfarin for 7 years past the date, stored in a drawer, and my INR hasn't budged. The FDA doesn't test for long-term stability because they don't want you to know how much money they're making off mandatory refills. You think your doctor cares? They get paid per visit, not per life saved. This whole 'NTI drug' thing is just a marketing ploy to keep you hooked on prescriptions.
Mussin Machhour
December 27, 2025 AT 22:41Bro this is so real. I had a buddy on lithium who used an expired bottle during a camping trip-thought he was fine till he started shaking like a leaf. Got rushed to the ER. Docs said his levels were half of what they should've been. Don't be that guy. Just get a new script. It's cheaper than an ambulance ride.
Justin James
December 28, 2025 AT 12:39Think about this: what if the expiration dates aren't about safety at all? What if they're a controlled obsolescence strategy by the pharmaceutical cartel? They know people won't question it because they're scared of dying. But here's the truth-most drugs don't degrade the way they claim. The real danger is the lack of transparency. The FDA doesn't release degradation data for NTI drugs because they're complicit. They're protecting profits, not patients. And don't get me started on how generics are forced into that 90-111% range-it's a loophole designed to make you pay more for the same chemical. They're playing chess with your life.
Winni Victor
December 28, 2025 AT 12:42Ugh. I hate when people act like expired meds are the end of the world. My grandma took her digoxin past the date for 11 years and still danced at my wedding. You people are so obsessed with control you forget humans survived for centuries without FDA-approved pill bottles. Also, who stores meds in a 'cool, dry place'? That's not a real room. That's a fantasy land where people don't live in bathrooms or cars or trailers. Chill. You're not a lab rat.
Linda B.
December 29, 2025 AT 08:18It is imperative to note, with the utmost gravity, that the assertion that degradation of NTI medications is benign is not only scientifically unfounded, but also morally reprehensible. The FDA’s 1985 study, while frequently cited, was conducted under laboratory conditions which do not reflect real-world storage environments-particularly in regions with high humidity and temperature fluctuations, such as the American South. To presume safety based on chemical stability alone is to commit a fallacy of composition. Furthermore, the absence of published case reports does not equate to absence of harm. It equates to underreporting. And underreporting, as we know, is systemic.
Christopher King
December 29, 2025 AT 11:58Okay but what if the real enemy isn't the expired pill-it's the system that makes you dependent on it? You think your doctor really wants you to be healthy? No. They want you to keep coming back. They want you to keep buying. They want you to fear your own body so much that you'll swallow anything they hand you. And now they've invented this 'narrow therapeutic index' nonsense to scare you into compliance. What if the 'danger' is manufactured? What if the whole thing is a psychological trap? I stopped taking my levothyroxine last year. I meditated more. I drank lemon water. My TSH is better than ever. Coincidence? Or awakening?
Michael Dillon
December 29, 2025 AT 16:58I get why this post matters, but let's be real-most people aren't taking these drugs for decades. You refill every 30 days. You check the date. You don't hoard pills like a prepper. The real issue is people who forget to refill and then grab whatever's left in the cabinet. That's the problem. Not the science. Not the degradation. Just human forgetfulness. Fix that, and you fix 90% of the risk.
Gary Hartung
December 31, 2025 AT 09:56One must acknowledge, with a profound sense of intellectual rigor, that the notion of 'expiration' as a regulatory construct is, in fact, a cultural artifact of late-stage pharmaceutical capitalism. The very term 'therapeutic index' implies a quantifiable boundary where none truly exists in biological systems-life is not a titration curve. To reduce human physiology to a 90-111% bioequivalence standard is to commit epistemic violence against the complexity of the organism. Furthermore, the insistence on 'original container storage' is a performative ritual designed to reinforce consumer dependence. I, for one, store my phenytoin in a glass vial beneath my bed, next to my crystals. The energy is better.
Jason Jasper
January 1, 2026 AT 05:30I appreciate the depth of this post. I’ve worked in a hospital pharmacy for 12 years and we treat NTI drugs like live grenades. We double-check every dose. We never dispense expired ones-even if the patient begs. I’ve seen what happens when someone takes an old warfarin pill. It’s not pretty. I’m not saying everyone needs to panic-but if you’re on one of these meds, treat it like your life depends on it… because it does.
Carlos Narvaez
January 2, 2026 AT 09:19Expired NTI drugs? Don’t use them. End of story. You don’t need a 10-page essay to understand that.
Harbans Singh
January 4, 2026 AT 07:36This is super important, especially in places like India where people often reuse old meds due to cost. I’ve seen relatives take leftover lithium after a hospital stay. They think, 'It worked before, so why not?' But their bodies change. Their kidneys change. The drug doesn't. We need more community education-not just warnings. Maybe local clinics could offer free disposal and low-cost refills. Small steps, big impact.
Zabihullah Saleh
January 5, 2026 AT 09:10You know, in my culture, we used to trust herbs and time. But this? This is different. This isn’t about tradition. It’s about precision. One molecule too little, and your heart forgets to beat. One too much, and your kidneys give up. It’s not magic. It’s math. And math doesn’t care if you’re broke or tired or skeptical. The pill either works or it doesn’t. And if it’s old? It’s not just weak-it’s a gamble with your next breath.
Rick Kimberly
January 5, 2026 AT 21:16While the article presents a compelling argument grounded in clinical pharmacology, it is imperative to recognize that the concept of 'expiration' is not universally standardized across jurisdictions. In the European Union, for instance, extended shelf-life studies are more commonly mandated for high-risk medications. Furthermore, the absence of degradation data for NTI drugs does not constitute evidence of instability-it constitutes a data gap. The appropriate response is not fear, but systematic research investment. To conflate regulatory caution with biological inevitability is a logical fallacy.
Terry Free
January 6, 2026 AT 12:36Wow. So let me get this straight. You're telling me that if I take a 3-year-old warfarin pill, I'm basically playing Russian roulette with my blood? And you want me to believe that the same company that gave me a 20% discount on my last refill is now suddenly my guardian angel? Yeah right. I'll keep taking it. If I die, I die. At least I didn't waste $120 on a new bottle.