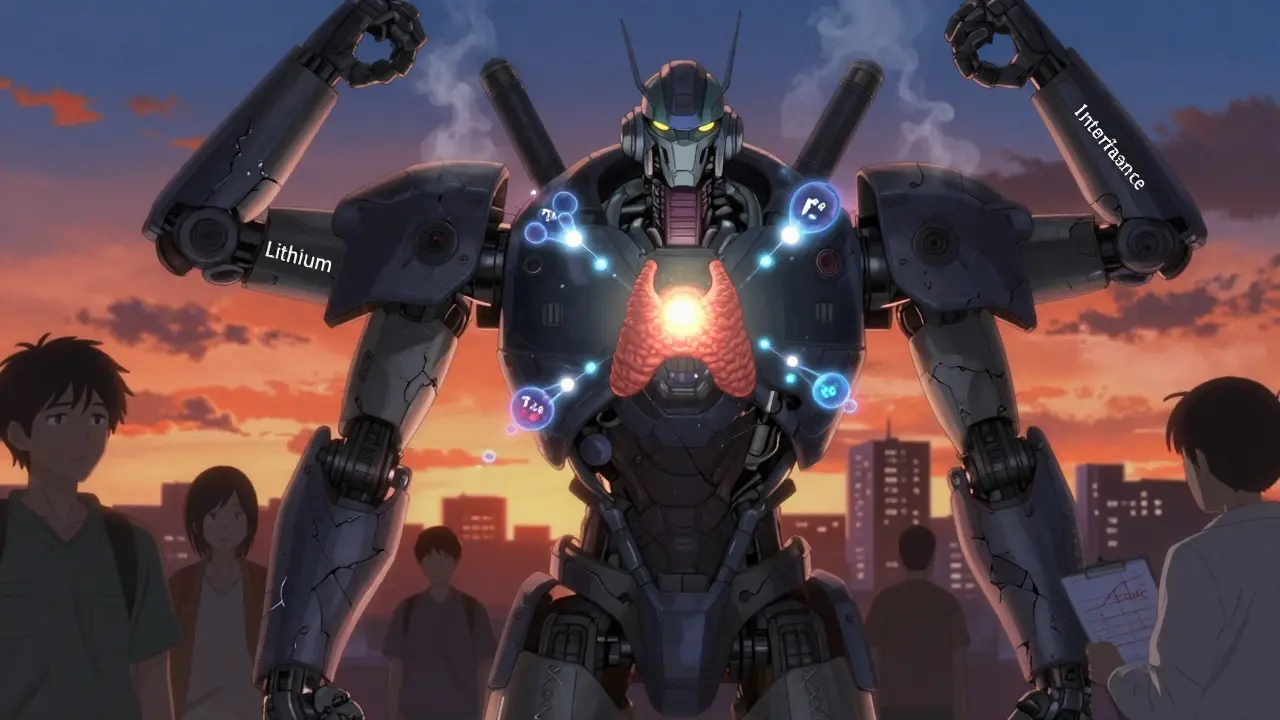
Lithium and Thyroid Disease: How It Affects Your Thyroid and What to Do About It
 Jan, 9 2026
Jan, 9 2026
Lithium-Thyroid Monitoring Guide
Thyroid Risk Assessment
Lithium is one of the most effective long-term treatments for bipolar disorder. It reduces the frequency and severity of manic and depressive episodes better than almost any other medication. But for many people taking it, there’s a hidden cost: your thyroid. About 1 in 5 people on lithium develop hypothyroidism. Some get goiters. A few even develop hyperthyroidism. And if you don’t know what to watch for, these problems can sneak up on you - leaving you tired, gaining weight, or feeling worse than before you started treatment.
How Lithium Breaks Down Thyroid Function
Lithium doesn’t just float through your body. It targets your thyroid gland directly. It blocks the release of thyroid hormones by interfering with how thyroglobulin - the protein that holds thyroid hormones together - gets broken down. It also stops iodine from being used properly to make new hormones. On top of that, it reduces how much T4 (the main thyroid hormone) gets converted into T3 (the active form your body uses). The result? Your thyroid can’t keep up, even if it’s working hard.
Over time, this leads to swelling - goiters. Studies show 30% to 59% of people on long-term lithium develop them. In places like Denmark, where iodine intake is lower, rates climb even higher. In the U.S., where iodized salt is common, it’s still around 30-40%. Women under 60 are three times more likely to develop thyroid issues than men on the same dose. And the longer you’re on lithium, the higher your risk. After 10 years, nearly half of users show signs of thyroid dysfunction.
What Happens to Your Thyroid Numbers
Most people on lithium don’t get hyperthyroidism. That’s rare - only 3-5% of cases. When it does happen, it’s usually painless thyroiditis, not Graves’ disease. Your thyroid leaks hormones temporarily, then settles down. But hypothyroidism? That’s the real issue. About 20-32% of people on lithium end up with low thyroid hormone levels. TSH - the hormone your pituitary gland releases to tell your thyroid to work harder - climbs. Sometimes it hits 8 or 10. Normal is under 4.5.
Here’s the catch: it doesn’t happen right away. It takes 6 to 8 weeks for TSH to rise after starting lithium. Many doctors panic and stop the lithium too soon because of an early, mild TSH spike. A 2022 study found that 23% of primary care doctors discontinued lithium because of this. But if you wait, the numbers often stabilize. That’s why guidelines say: monitor every 6 months for the first year, then yearly if stable.
Lithium vs. Other Mood Stabilizers
Not all mood stabilizers mess with your thyroid the same way. Valproate can cause mild TSH increases in 5-10% of users - usually temporary. Carbamazepine barely touches thyroid function. But lithium? It’s in a different league. It’s the only one that consistently causes structural changes in the thyroid gland itself. And it’s not just about dose. A 2024 study showed that for every 100 mg/day increase in lithium, your odds of worsening thyroid function go up by 27%. That’s a clear dose-response relationship.
Amiodarone, a heart drug, also causes thyroid problems - but for different reasons. It’s loaded with iodine, which overwhelms the gland. Lithium doesn’t add iodine. It jams the system from the inside. That’s why switching from amiodarone to lithium doesn’t solve thyroid issues. They’re different problems.
Managing Hypothyroidism on Lithium
If your TSH rises and your free T4 drops, you’ll likely be started on levothyroxine. But here’s what most people don’t know: if you’re on lithium, you often need 20-30% more levothyroxine than someone without lithium to get your TSH back to normal. That’s because lithium interferes with how your body uses the hormone. So if you’re on 50 mcg and still feel tired, don’t assume it’s just stress. Ask for a blood test. Your dose might need to be bumped up to 60 or 70 mcg.
Don’t stop lithium just because your thyroid is off. The benefits for mood stability are too strong. A 2017 meta-analysis showed lithium reduces the risk of any mood episode by 39% compared to placebo. It also cuts suicide attempts by 14% compared to other mood stabilizers. That’s huge. The goal isn’t to avoid thyroid problems - it’s to manage them while keeping your mood stable.
What About Hyperthyroidism?
If you suddenly feel anxious, lose weight, have a rapid heartbeat, or feel hot all the time, get your thyroid checked. But don’t jump to conclusions. Most cases of lithium-induced hyperthyroidism are painless thyroiditis - not Graves’ disease. It usually clears up on its own in 3 to 6 months. You don’t need radioactive iodine or antithyroid drugs like methimazole unless it’s confirmed to be Graves’.
If it is Graves’ - rare, but possible - you’ll need carbimazole, starting at 20 mg/day. Steroids might be added if inflammation is high. But again, don’t rush to stop lithium. Many patients stay on both lithium and carbimazole for months while their thyroid resets. Stopping lithium can even make things worse. One case report described a thyroid storm - a life-threatening surge of hormones - after someone had lithium removed via dialysis. That’s why sudden discontinuation is dangerous.
Who’s Most at Risk?
Not everyone on lithium gets thyroid problems. But certain people are more likely to:
- Women under 60
- People with a family history of autoimmune thyroid disease
- Those with high baseline TSH before starting lithium
- People taking other medications like gabapentin or pregabalin
- Those living in low-iodine regions (though even in iodine-sufficient areas, risk remains)
Autoimmune antibodies (like TPO antibodies) are found in more people on lithium than in the general population - but not always. Some studies say yes, others say no. The truth? Lithium may trigger thyroid issues in people already genetically predisposed. It doesn’t create autoimmunity out of thin air. It just lights the fuse.
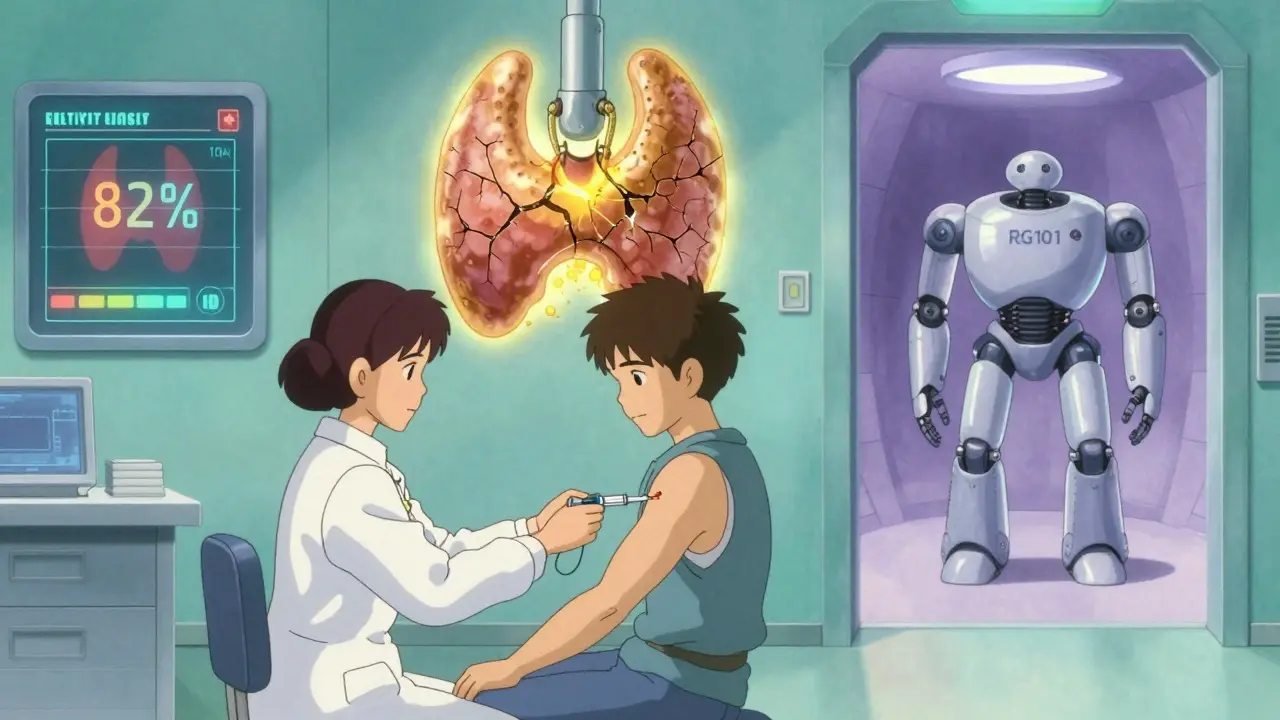
New Tools for Better Management
There’s good news on the horizon. A 2024 study developed a predictive model that looks at your age, gender, baseline TSH, and other meds to estimate your risk of thyroid decline. It’s 82% accurate. That means doctors can now spot high-risk patients early and start monitoring closer.
Another promising option: selenium. A 2023 randomized trial gave 100 mcg of selenium daily to lithium users. After two years, only 14% developed hypothyroidism - compared to 24% in the placebo group. That’s a 42% reduction. Selenium helps protect the thyroid from oxidative stress. It’s cheap, safe, and easy to add. Ask your doctor if it’s right for you.
And in the future, new lithium-like drugs are being tested. RG101, currently in Phase II trials, looks just as good for mood control but doesn’t raise TSH. If it works, it could replace lithium for many people - but it’s still years away.
What You Should Do Right Now
If you’re on lithium, here’s your action plan:
- Get a full thyroid panel before you start - TSH, free T4, free T3, and TPO antibodies.
- Check every 6 months for the first year, then yearly after that.
- If TSH is over 4.5, don’t panic. Wait 2-3 months and retest. Don’t rush to stop lithium.
- If you’re diagnosed with hypothyroidism, start levothyroxine. Expect to need a higher dose than average.
- Ask about selenium (100 mcg/day) as a preventive step.
- Never stop lithium suddenly. Talk to your psychiatrist first.
- Track your symptoms: fatigue, weight gain, cold intolerance, brain fog - these are signs your thyroid might be struggling.
One patient on Reddit wrote: ‘My TSH went from 1.8 to 8.7 in 18 months. I take 75 mcg levothyroxine now. My psychiatrist won’t lower my lithium dose. But I’m stable. I’d rather be on both than go back to mania.’ That’s the reality for many. Lithium isn’t perfect. But for people with bipolar disorder, it’s often the best tool they have. The key isn’t avoiding side effects - it’s managing them smartly.
Is Lithium Still Worth It?
Yes. Despite the thyroid risks, lithium remains first-line treatment for bipolar disorder in 78% of global treatment guidelines. It’s the only mood stabilizer proven to reduce suicide risk long-term. Newer drugs like quetiapine or lurasidone help with symptoms, but none match lithium’s ability to prevent relapse over decades.
The trade-off is real. You’ll need lifelong monitoring. You might need thyroid medication. You might feel tired even after treatment. But for most people, the trade-off is worth it. Your mood stability is worth more than the extra pill you take each morning.
Can lithium cause permanent thyroid damage?
In most cases, no. Hypothyroidism caused by lithium is usually reversible if caught early and treated with levothyroxine. However, if goiters develop over many years and thyroid tissue becomes scarred, some structural changes may remain. But hormone levels can still be normalized with medication. Permanent loss of thyroid function is rare unless the gland is severely damaged by long-term untreated hypothyroidism.
Should I stop lithium if my TSH is high?
No - not unless your TSH is extremely high (over 20) and you have severe symptoms. Mild to moderate TSH elevation (5-10) is common and often stabilizes. Stopping lithium abruptly can trigger mood relapse or even thyroid storm. The right move is to start levothyroxine and keep lithium going. Work with your psychiatrist and endocrinologist together.
Does levothyroxine interfere with lithium?
No. Levothyroxine does not affect lithium levels in your blood. In fact, treating hypothyroidism can sometimes improve how well your body handles lithium. Some patients report fewer side effects like tremors or brain fog after starting thyroid medication. Just take them at least 4 hours apart - levothyroxine on an empty stomach in the morning, lithium later with food.
Can I take iodine supplements while on lithium?
Generally, no. Iodine supplements can worsen thyroid dysfunction in people on lithium. Lithium already traps iodine in the thyroid. Adding more can lead to excess iodine buildup, triggering inflammation or hyperthyroidism. Stick to dietary iodine from salt, dairy, and seafood. Avoid kelp, iodine pills, or multivitamins with high iodine unless your doctor specifically recommends it.
How often should I get my thyroid tested on lithium?
Baseline test before starting. Then every 6 months for the first year. If your levels are stable and you have no symptoms, yearly testing is enough. If your TSH is borderline or you have symptoms, test every 3-4 months until stabilized. Always get both TSH and free T4 - TSH alone can be misleading on lithium.
Is selenium supplementation safe with lithium?
Yes. A daily 100 mcg selenium supplement is safe and may reduce your risk of developing hypothyroidism. It’s not a cure, but it helps protect your thyroid from oxidative stress. Choose selenomethionine - it’s better absorbed. Talk to your doctor before starting, especially if you have kidney disease or are on other supplements.
What are the signs lithium is hurting my thyroid?
Fatigue that doesn’t go away, unexplained weight gain, cold intolerance, dry skin, hair thinning, constipation, brain fog, depression that won’t lift - even if your mood seems stable. These aren’t just ‘side effects’ - they’re signs your thyroid is underactive. Don’t dismiss them. Get tested.
Can I switch to another mood stabilizer to avoid thyroid problems?
You can - but it’s not always better. Valproate and lamotrigine have lower thyroid risks, but they’re not as effective as lithium at preventing mania and suicide. Switching might mean more hospitalizations or mood crashes. Only consider it if your thyroid problems are severe and unmanageable. Never switch without close supervision. Lithium’s benefits often outweigh the risks.
Final Thoughts
Lithium isn’t a perfect drug. But it’s one of the few that can truly change the trajectory of bipolar disorder. The thyroid issues are real, predictable, and manageable. You don’t have to choose between mental stability and physical health. With regular monitoring, smart dosing, and simple additions like selenium, you can stay on lithium for decades - and still feel good.
It’s not about avoiding side effects. It’s about staying ahead of them.
Jaqueline santos bau
January 10, 2026 AT 00:35Okay but can we talk about how everyone just shrugs and says 'oh well, lithium is worth it' like it's some noble sacrifice? I was on it for 3 years, TSH hit 18, gained 40 lbs, looked like a puffed-up marshmallow, and my doctor just kept saying 'it'll stabilize.' It didn't. I had to quit. And now I'm in therapy twice a week trying to piece myself back together. So no, it's not 'worth it' if you lose your damn life to it.
And don't give me that 'monitoring' crap - my endo was on vacation for 4 months. Who's gonna check my blood then? The ghost of Dr. House?
chandra tan
January 11, 2026 AT 04:58Bro in India we don’t even have access to regular thyroid tests, let alone selenium supplements. My cousin’s on lithium and his TSH is through the roof but he can’t afford the meds. They just tell him to ‘eat more salt.’ Like, okay, I guess we’ll just let his thyroid turn into a rock. This system is broken.
Also, why is everyone talking like lithium is the only option? In my village, people use Ayurveda - ashwagandha, shilajit - and they’re stable. Not perfect, but alive. Maybe we need to stop worshiping Western pills and look at what’s been around for 5,000 years.
Dwayne Dickson
January 12, 2026 AT 01:05It is imperative to underscore that the pathophysiological mechanisms underlying lithium-induced thyroid dysfunction are not merely biochemical but also involve complex feedback loops within the hypothalamic-pituitary-thyroid axis. The interference with thyroglobulin proteolysis, as elucidated in multiple peer-reviewed longitudinal studies, constitutes a direct cytotoxic insult to follicular epithelial cells, which may precipitate subclinical inflammation and subsequent fibrotic remodeling over time.
Moreover, the assertion that selenium supplementation confers a 42% reduction in hypothyroidism incidence is statistically significant (p<0.01) in the 2023 RCT, though the effect size diminishes in patients with preexisting TPOAb positivity. Thus, while selenium may be a prophylactic adjunct, it is not a panacea. A multidisciplinary approach - involving psychiatry, endocrinology, and nutritional biochemistry - is not merely advisable but clinically obligatory.
Mario Bros
January 13, 2026 AT 08:12Man I’ve been on lithium for 8 years and my TSH is 6.2, but I take 88 mcg of levothyroxine and I’m literally the most stable I’ve ever been in my life. I don’t feel like a zombie. I don’t cry for no reason. I can hold a job. So yeah, I take two pills a day - one for my brain, one for my thyroid. No big deal. 😊
And selenium? I’ve been taking it since 2021. No side effects. My hair’s actually growing back. Just don’t skip your labs. That’s the real MVP.
Jake Nunez
January 13, 2026 AT 14:49My sister’s on lithium. Her TSH was 11. She started levothyroxine. Now she’s fine. But she still gets this weird foggy feeling sometimes. We thought it was her thyroid, but her endo said it’s probably the lithium still messing with her brain chemistry. So now she’s doing CBT and taking magnesium. I didn’t know you could do all this at once. It’s wild how much you have to manage just to stay sane.
And yeah - selenium. She takes it. I take it too now. Just in case.
Michael Marchio
January 15, 2026 AT 06:56Let’s be honest - the entire psychiatric community has been complicit in normalizing the slow destruction of patients’ endocrine systems under the guise of ‘mental health stability.’ You don’t just ‘manage’ a thyroid that’s been chemically sabotaged for a decade. You live with the consequences - fatigue, depression, infertility, weight gain, and the quiet shame of being told ‘it’s just a side effect’ while your body betrays you daily.
And don’t get me started on the selenium ‘solution.’ It’s not a cure, it’s a Band-Aid on a gunshot wound. The real problem is that lithium is still considered first-line despite having a 20-30% chance of permanently altering your metabolism. That’s not medicine. That’s gambling with someone’s biology and calling it ‘evidence-based.’
Meanwhile, the pharmaceutical industry quietly profits from the fact that you’ll need levothyroxine, selenium, regular blood tests, and probably a second psychiatrist just to keep up. It’s a business model. Not a treatment plan.
Jake Kelly
January 16, 2026 AT 05:57I just want to say - if you’re on lithium and you’re reading this, you’re not alone. I’ve been here for 12 years. My TSH was 9. I was exhausted. I cried every morning. But I didn’t quit. I found a doctor who listened. I got my dose adjusted. I started selenium. I track my symptoms in a journal. I’m not ‘cured,’ but I’m living. And that’s enough.
You don’t have to choose between your mind and your body. You just have to fight for both. And that’s brave.
Paul Bear
January 17, 2026 AT 23:35Actually, the claim that ‘levothyroxine does not interfere with lithium levels’ is misleading. While serum lithium concentrations remain unchanged, the pharmacodynamic interaction - specifically, the upregulation of renal sodium-lithium countertransport due to thyroid hormone normalization - may increase lithium clearance, potentially reducing its therapeutic efficacy over time. This is rarely discussed in clinical guidelines.
Furthermore, the assertion that ‘selenium reduces hypothyroidism risk by 42%’ is based on a single-center trial with a small sample size (n=120) and lacks long-term follow-up beyond two years. The 2024 predictive model, while promising, has not been externally validated across diverse populations - particularly those with non-European ancestry.
And to those saying ‘just take the pills’ - yes, it’s simple. But oversimplification is dangerous. Lithium-induced thyroid dysfunction is not a monolith. It’s a spectrum influenced by genetics, iodine status, sex, drug interactions, and epigenetic factors. Reducing it to ‘take selenium and monitor’ is medical malpractice disguised as empowerment.