Insulin Safety: Mastering Dosing Units, Syringes, and Preventing Hypoglycemia
 Dec, 21 2025
Dec, 21 2025
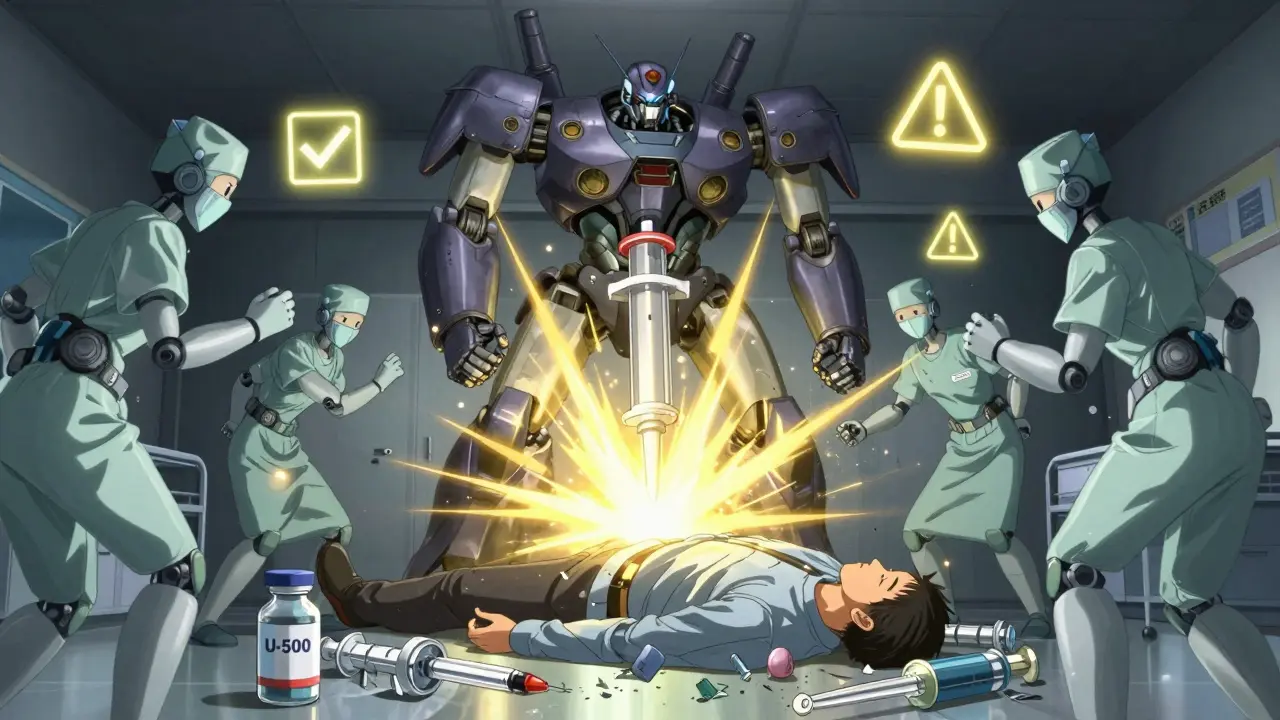
Getting insulin dosing wrong isn’t just a mistake-it can land you in the hospital. One extra unit, the wrong syringe, or a miscalculated carb ratio can send blood sugar crashing. And it’s not rare. Studies show that insulin dosing errors are among the most common and dangerous medication mistakes in diabetes care. You’re not alone if you’ve ever stared at your pen, wondering if you got it right. But here’s the truth: with clear rules, the right tools, and a few key habits, you can avoid the biggest risks.
Understanding Insulin Concentration: U-100 vs. U-500
Not all insulin is the same. Most people use U-100 insulin-that’s 100 units per milliliter. It’s the standard for pens, vials, and syringes. But some people with severe insulin resistance need U-500, which is five times stronger. That’s 500 units in the same space. Mixing them up is deadly. If you think you’re giving 10 units of U-100 but grab a U-500 vial instead, you’ve just given 50 units. That’s a massive overdose. Always check the label. Always. Even if you’ve used the same insulin for years. Labels change. Vials look similar. Never assume.The Syringe That Could Save Your Life
Insulin syringes aren’t like regular ones. They’re marked in units, not milliliters. And they’re designed to match the insulin you’re using. A U-100 syringe holds exactly 100 units per mL. If you use a U-100 syringe with U-500 insulin, you’ll give five times the dose you think you are. Same problem the other way around. Use the right syringe. Always. There’s no exception. Even if you’re in a hurry, even if you’re tired. Your life depends on this detail.And don’t reuse syringes. Yes, some people do it to save money. But reusing needles increases infection risk, blunts the tip, and makes injections painful and inaccurate. A dull needle doesn’t deliver the full dose. It can also damage tissue. Buy new ones. If cost is an issue, talk to your doctor. There are programs that help.
How Much Insulin Should You Really Take?
There’s no one-size-fits-all dose. But there are starting points. For someone new to insulin, doctors often begin with 0.1 to 0.2 units per kilogram of body weight. So if you weigh 70 kg (about 154 lbs), that’s 7 to 14 units total per day. That’s usually split-some for meals, some for background control.Basal insulin (like Lantus, Basaglar, or Tresiba) is given once or twice daily to keep blood sugar steady between meals and overnight. A common starting dose is 10 units once a day, or 0.2 units per kg. If you’re switching from another insulin, like NPH, you’ll usually reduce your dose by 20%. For example, if you were on 60 units of NPH, you’d start with 48 units of Lantus. Why? Because long-acting analogs are more predictable and don’t have the peak NPH does. Too much can cause low blood sugar.
For mealtime insulin (rapid-acting like Humalog, NovoLog, or Fiasp), you need two numbers: your carb ratio and your correction factor. The carb ratio tells you how many grams of carbs one unit of insulin covers. Most people start with 1 unit per 10-15 grams of carbs. The Rule of 500 helps: divide 500 by your total daily insulin dose. So if you take 40 units a day, 500 ÷ 40 = 12.5. That means one unit covers about 12.5 grams of carbs.
The correction factor tells you how much one unit lowers your blood sugar. The Rule of 1800 applies here: divide 1800 by your total daily insulin. So again, if you take 40 units, 1800 ÷ 40 = 45. That means one unit drops your blood sugar by about 45 mg/dL. If your reading is 220 and your target is 100, you’re 120 points high. 120 ÷ 45 = 2.67. So you’d take about 3 units to correct it.
The Hidden Math Trap: Insulin Conversion Errors
Here’s something most people don’t know. There’s a scientific error hiding in plain sight. Insulin is measured in units (U), which reflect biological effect-not weight. But some lab reports and online calculators use the wrong conversion factor to turn units into mass. The correct factor is 5.18 (meaning 1 unit = 5.18 pmol of insulin). But many systems use 6.0. That’s a 15% error. It sounds small, but in research and dosing algorithms, it adds up. If your doctor’s software uses the wrong number, your calculated dose could be off. That’s why you should never rely on random apps or websites for insulin math. Always double-check with your care team. Ask them: “Are you using the correct conversion factor?”
Hypoglycemia: The Silent Danger
Low blood sugar is the biggest fear for anyone on insulin. It can sneak up fast. Symptoms? Sweating, shaking, confusion, dizziness, rapid heartbeat. If you ignore it, you can pass out-or worse. Always carry fast-acting sugar: glucose tablets, juice, or candy. Don’t wait until you feel bad. Check your blood sugar if you feel off. Even if you think it’s just stress or tiredness.Some people get hypoglycemia unawareness. That means they don’t feel the warning signs. This is dangerous. If that’s you, talk to your doctor. You might need to adjust your target range slightly higher for a while. Or use a continuous glucose monitor (CGM). CGMs beep when your sugar drops, even while you’re sleeping. They’ve changed lives.
And never skip meals after taking mealtime insulin. If you eat less than planned, your insulin will still be working. Blood sugar plummets. That’s why carb counting matters. If you planned for 60 grams of carbs but only ate 30, you’re at risk. Always match insulin to food. If you’re unsure, underdose. You can always correct later. But once you’re low, it’s harder to climb back up.
When You Switch Insulins: What You Must Know
Switching from one insulin to another isn’t just swapping bottles. Each type acts differently. Lantus and Basaglar are similar, but switching from NPH to Lantus? Cut your dose by 20%. Tresiba is longer-lasting than Basaglar. If you switch from Tresiba to Basaglar and were taking 100 units once daily, you’ll need to split it-maybe 40 units twice a day. That’s 80% of your original dose. Don’t guess. Follow your provider’s exact instructions.After switching, check your blood sugar more often-for at least two weeks. Your body is adjusting. You might need small tweaks. Don’t rush to change your dose. Wait a few days between adjustments. And always write down your readings. Patterns matter more than single numbers.
Real-Life Example: A Meal Dose in Action
Let’s say you’re taking 40 units of insulin total per day. Your carb ratio is 1 unit per 12.5 grams. Your correction factor is 45 mg/dL per unit. You plan to eat a meal with 90 grams of carbs. Your blood sugar is 210 mg/dL. Target is 100.- Carb dose: 90 ÷ 12.5 = 7.2 units → round to 7 units
- Correction dose: (210 - 100) = 110 ÷ 45 = 2.44 → round to 2.5 units
- Total: 7 + 2.5 = 9.5 units → round to 10 units
You give 10 units. You eat. You wait. You check again in 2 hours. That’s how it’s done. Not guesswork. Not memory. Math.
What to Do If You Mess Up
You gave too much insulin? You forgot to eat? You took insulin and then went for a walk and didn’t realize you were low? Here’s what to do:- Check your blood sugar immediately.
- If it’s below 70 mg/dL, take 15 grams of fast-acting sugar (4 glucose tablets, ½ cup juice, or 1 tablespoon honey).
- Wait 15 minutes. Check again.
- If still low, repeat.
- If you’re confused, dizzy, or can’t swallow, someone else must give you glucagon or call 911.
Glucagon kits are available by prescription. Make sure your family, friends, or coworkers know how to use one. Keep it in your bag, your car, your desk. You never know when you’ll need it.
Final Tip: Write It Down
Use a notebook or app to log:- Your blood sugar before and after meals
- Your insulin doses (type, units, time)
- What you ate (especially carbs)
- Exercise, stress, illness
Patterns reveal the truth. If your sugar is low every Tuesday after lunch, maybe your carb ratio is too high. If it’s high every morning, maybe your basal dose needs tweaking. Data beats guesswork. And your doctor needs this to help you.
Insulin is powerful. It can save your life. But only if you use it safely. Don’t let confusion or haste turn a lifesaving tool into a danger. Know your numbers. Use the right syringe. Check your labels. Always. You’ve got this.
Can I use the same syringe for U-100 and U-500 insulin?
No. Never. U-500 insulin is five times stronger than U-100. Using a U-100 syringe with U-500 insulin will deliver five times the dose you intend. Always use a syringe labeled for the specific insulin concentration. Some manufacturers make special syringes for U-500-ask your pharmacist.
How do I know if I’m taking too much insulin?
Frequent low blood sugar (below 70 mg/dL), especially without a clear cause like skipping a meal or exercising, is a red flag. You might also notice unexplained weight gain, constant fatigue, or needing more carbs to stay out of low. If this happens, review your doses with your provider. Your carb ratio or correction factor may be too aggressive.
Is it safe to adjust my insulin dose on my own?
Small, planned adjustments are usually safe if you’ve been trained. For example, adding 1-2 units to your basal insulin if your fasting sugar is above 130 mg/dL for 3 days in a row is common. But never change your dose by more than 10% at a time without guidance. If you’re unsure, call your doctor. Too much change can cause dangerous lows.
Why do some people need U-500 insulin?
People with severe insulin resistance-often due to obesity, long-standing Type 2 diabetes, or certain medical conditions-need very high doses. Giving 100+ units of U-100 insulin daily means multiple injections and large volumes. U-500 allows them to take the same dose in a smaller volume, making it easier and more accurate.
Can I use a pen injector instead of a syringe?
Yes, for most people, pens are easier and more accurate. But make sure your pen matches your insulin type and concentration. Some pens only work with specific insulins. Never use a pen with insulin it wasn’t designed for. Also, pens can’t be used with U-500 insulin-only syringes are approved for that.
How often should I check my blood sugar when starting insulin?
When you first start insulin, check at least 4 times a day: before each meal and at bedtime. That gives you enough data to see how your body responds. After a few weeks, if things are stable, you might reduce to 2-3 times daily. But always check more often if you’re sick, stressed, or changing your routine.
What should I do if I miss a dose of basal insulin?
If you miss your basal insulin and it’s been less than 2 hours, take your usual dose. If it’s been longer, don’t double up. Check your blood sugar. If it’s high, use your correction factor for a small dose. If you’re unsure, call your doctor. Missing one dose won’t cause an emergency, but repeated misses can lead to complications.
Can alcohol affect my insulin dose?
Yes. Alcohol can delay low blood sugar for hours-even up to 24 hours after drinking. It blocks your liver from releasing glucose. If you drink, eat carbs with it. Check your blood sugar before bed. Consider reducing your evening insulin if you’ve had alcohol. Never drink on an empty stomach.
Next Steps: What to Do Today
- Check your insulin labels right now. Are you sure you’re using the right concentration?
- Verify your syringe type. Is it matched to your insulin?
- Review your last 7 days of blood sugar logs. Look for patterns of lows or highs.
- If you’re unsure about your carb ratio or correction factor, write down your total daily insulin and calculate them using the 500 and 1800 rules.
- Ask your doctor or pharmacist: "Am I using the correct insulin conversion factor in my dosing plan?"
Insulin safety isn’t about perfection. It’s about awareness. One small habit-like checking the label-can prevent a hospital visit. You’re not just managing diabetes. You’re protecting your future. Do it right.
Charles Barry
December 23, 2025 AT 10:44Let me guess-your ‘doctor’ is using the wrong conversion factor (6.0 instead of 5.18) and you’re getting dosed wrong by 15% every time. This isn’t incompetence, it’s systemic. Big Pharma wants you dependent. They’ve known about this for decades. The FDA? Complicit. You think your CGM saves you? Nah. It’s just feeding data into their algorithm to adjust your dose *just enough* to keep you alive but never stable. Wake up. They profit from your chaos.
Rosemary O'Shea
December 24, 2025 AT 00:02Oh please. You’re all acting like this is some groundbreaking revelation. I’ve been managing Type 1 since 1998. The U-100/U-500 mix-up? That’s Diabetes 101. And the 500/1800 rule? Cute. But real clinicians use insulin sensitivity factors derived from *actual* glucose curves, not some 1980s math parlor trick. You’re not ‘mastering’ dosing-you’re clinging to outdated heuristics while ignoring personalized pharmacokinetics. If your doctor still uses the Rule of 500 without a CGM trend analysis, find a new one.
Kathryn Weymouth
December 25, 2025 AT 18:39I appreciate the thorough breakdown, but I’m concerned about the phrasing around insulin conversion factors. The value of 5.18 pmol/unit is correct for human insulin, but it’s not universally applied in clinical software because most systems use insulin mass in *micrograms*, not picomoles. The 6.0 factor is often used because it approximates 6.0 µg/unit (based on molecular weight), which is simpler for dosing algorithms. The 15% error claim is misleading-it’s not an error if the system is designed consistently. What matters is internal consistency, not arbitrary biochemical precision. Always confirm your clinic’s protocol, but don’t assume they’re wrong just because the number differs from a research paper.
Nader Bsyouni
December 27, 2025 AT 03:49Why do we even use units anyway Why not just milligrams Like everything else in medicine Why is insulin this magical exception Who decided that and why Are we still living in the 1920s What if the whole system is just a relic of old-school biochemistry and we’re all just playing along because no one wants to admit it’s a mess
Julie Chavassieux
December 28, 2025 AT 08:22U-500... syringes... labels... I just... I can’t... I had a panic attack reading this. I’m 23 and I’ve been on insulin since I was 8. I’ve used the same pen for three years. I didn’t even know U-500 existed. What if I’ve been doing it wrong this whole time? I’m not even mad. I’m just... hollow. Someone please tell me I’m not going to die tomorrow.
Ajay Brahmandam
December 30, 2025 AT 04:02Bro this is solid info. I’ve been on insulin for 12 years and I never knew about the 5.18 vs 6.0 thing. I always just trusted my app. Now I’m gonna ask my doc tomorrow. Also-don’t reuse needles. I used to do it to save cash. Bad idea. My skin looks like a pincushion. New needles cost like 20 cents each. Worth every penny. Stay safe out there.
Aliyu Sani
December 30, 2025 AT 07:22Y’know… insulin ain’t just chemistry-it’s power. It’s control. It’s the difference between living and just existing. When you’re in a country where insulin costs more than rent, you don’t just ‘dose right’-you survive right. The math? It’s a luxury. The label check? That’s survival instinct. I’ve seen people swap vials because the labels peeled off. They didn’t know. They just needed to live. This post is academic. But real life? It’s messy. We need access, not just algorithms.
Herman Rousseau
December 31, 2025 AT 13:38This is the kind of post that makes me want to hug everyone with diabetes. Seriously. You’re doing the math, checking the labels, logging your numbers-this is heroic. Don’t let anyone make you feel like you’re overdoing it. Safety isn’t paranoia-it’s power. And if you’re reading this and thinking ‘I’m not good enough’-you are. Keep going. You’re not alone. 💪❤️
jenny guachamboza
January 1, 2026 AT 12:54Wait so U-500 is 5x stronger??? So like… if I used my U-100 pen with U-500… I just gave myself a heart attack?? 😱 I’m gonna check my insulin right now. Also I think my doctor is part of the conspiracy. Why else would they keep giving me the same dose when I’m always low?? #InsulinGate #BigPharmaLies
Kiranjit Kaur
January 3, 2026 AT 09:00Thank you for writing this. I’m 67 and I just started insulin last year. I was terrified. But reading this made me feel like I could actually understand it. I wrote down my carb ratio and correction factor using the 500/1800 rule. My sugar’s been better since. I even showed my grandson. He’s 10. He said ‘Grandma, you’re a scientist now.’ 😊
Sai Keerthan Reddy Proddatoori
January 5, 2026 AT 06:27Western medicine always overcomplicates things. In my village, we used to eat neem leaves and bitter gourd. No syringes. No units. No apps. Just nature. Now you people pay thousands for pens and CGMs. This is not healing. This is dependency. You think you’re safe? You’re just buying into a system that profits from your fear. Go back to roots. Stop trusting the lab.
Cara Hritz
January 5, 2026 AT 16:47Wait so if I used a U-100 syringe with U-500 insulin I gave myself 5x the dose?? I think I did that once last year?? I’m gonna die??
Johnnie R. Bailey
January 5, 2026 AT 18:04That last comment? That’s why we need to talk about this. Not just the math. Not just the syringes. But the fear. The shame. The loneliness. I’ve been on insulin for 22 years. I’ve had lows so bad I peed my pants in a parking lot. I’ve cried over a glucometer. I’ve hidden my pens from my kids because I didn’t want them to be scared. This post? It’s not just information. It’s a lifeline. And if you’re reading this and you’re scared? You’re not broken. You’re human. And you’re not alone. I’ve been there. Keep going. One unit at a time.