Medical Tourism and Medication Safety: What You Must Know Before You Travel
 Jan, 4 2026
Jan, 4 2026
Why Medical Tourism Is Growing-And Why It’s Riskier Than You Think
More than 14 million people travel abroad each year for medical care. They’re drawn by lower prices, shorter wait times, and access to treatments not available at home. A knee replacement in Thailand might cost $10,000 instead of $50,000 in the U.S. A hair transplant in Turkey can be 70% cheaper than in Germany. Dental work in Mexico saves patients thousands. But behind the savings is a hidden risk: medication safety.
Most people focus on hospital ratings, surgeon credentials, and price tags. Few ask: What’s in the pills I’m given? Will my home doctor even recognize them? Can I refill them when I get back? These aren’t just minor concerns-they’re life-or-death questions.
The Real Cost of Cheap Care: Medication Gaps You Can’t Afford to Ignore
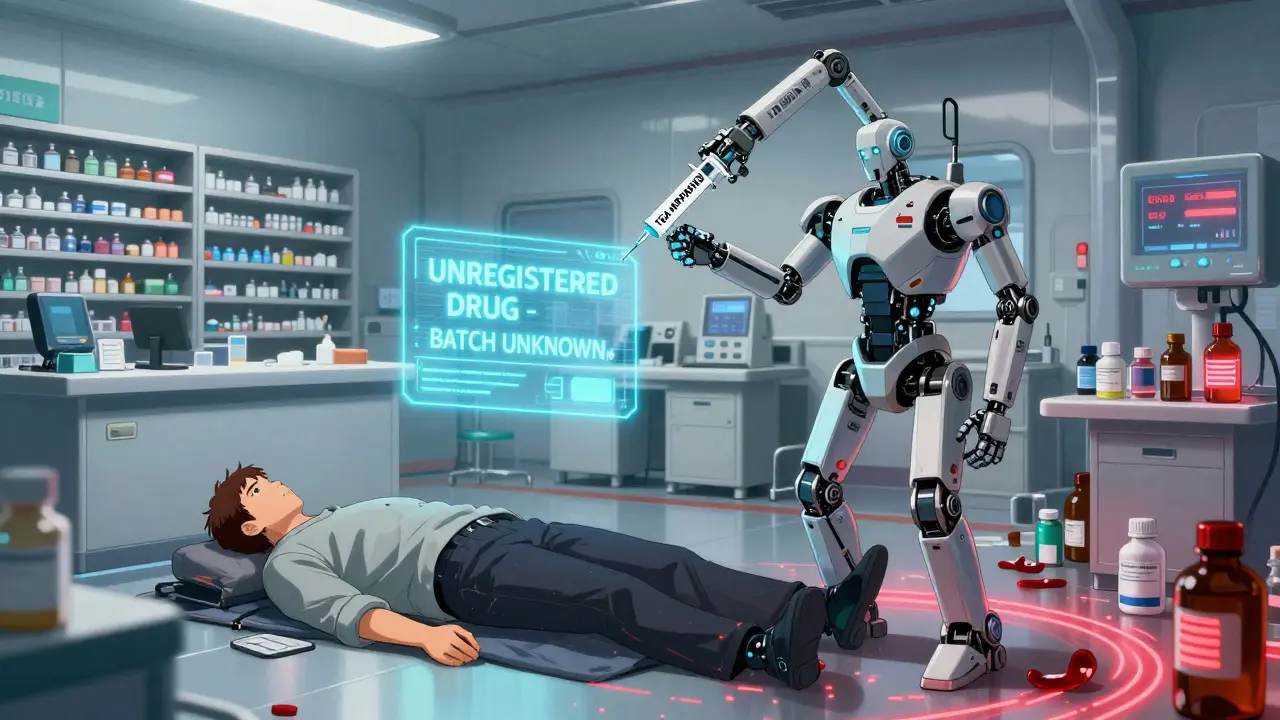
Imagine this: You get a hip replacement in India. The hospital gives you a powerful painkiller, an antibiotic, and a blood thinner. You fly home two weeks later. Your doctor in Melbourne checks your chart and says, “I’ve never heard of these drugs.”
That’s not rare. In fact, it’s common.
Medications approved in one country may be banned, untested, or simply unavailable in another. A drug labeled “Celecoxib” in the U.S. might be sold as “Celcoxx” in Thailand-with a different filler, dose, or manufacturer. Some pills sold abroad are counterfeit. The World Health Organization estimates 1 in 10 medical products in low- and middle-income countries are substandard or fake. That means you could be taking a pill with no active ingredient… or worse, a toxic one.
Even if the drug is real, the dosage might be wrong for your body. Genetic differences, weight, liver function-all these affect how drugs work. A dose that’s safe in South Korea might be dangerous for you in Australia. And if you’re on other medications back home? That’s a recipe for dangerous interactions.
How Regulatory Chaos Creates Medication Nightmares
There’s no global standard for drug approval. The U.S. FDA, the European EMA, and Australia’s TGA have strict rules. But in some countries, the process is looser-or poorly enforced.
For example:
- Antibiotics are sold over the counter in some countries without a prescription-leading to misuse and antibiotic resistance.
- Some clinics in Turkey and Mexico use drugs approved by the EU, which are closer to Western standards. But even then, storage conditions aren’t always monitored.
- In parts of Southeast Asia, medications are often imported without proper tracking, making it impossible to trace recalls or contamination.
And here’s the kicker: When you return home, your doctor has no way to verify what you were given. No barcode. No batch number. No electronic record. You’re left guessing whether that blue pill you took was the real thing.
What JCI Accreditation Doesn’t Tell You
Many medical tourism agencies push JCI (Joint Commission International) accreditation like a seal of approval. And yes, JCI hospitals usually have better infrastructure, cleaner facilities, and trained staff.
But JCI doesn’t guarantee medication safety.
It checks if the hospital has a pharmacy. It checks if staff follow basic protocols. But it doesn’t audit drug sourcing, track counterfeit risks, or require cross-border compatibility with your home country’s drug list. A hospital can be JCI-accredited and still give you a medication your doctor can’t refill, or one that’s been sitting in a hot warehouse for months.
Don’t confuse cleanliness with safety. A sparkling operating room doesn’t mean your pills are safe.

What You Need to Do Before You Book Your Flight
Here’s what actually works-not fluff, not marketing. Real steps:
- Talk to your doctor before you go. Bring a full list of your current medications. Ask: “What if I get prescribed something new? Can we get equivalents here?”
- Ask for the generic name, not the brand. If you’re given “CardiMax,” ask for “Clopidogrel.” That’s the active ingredient. It’s the same everywhere.
- Request the manufacturer and batch number. Write it down. Take a photo of the pill bottle. If something goes wrong, this is your only proof.
- Check if your home country recognizes the drug. Use your national drug database (like TGA’s in Australia or FDA’s in the U.S.) to search the generic name. If it’s not listed, you’re on your own.
- Get a written discharge summary. It should include every drug given, dosage, frequency, and reason. No excuses. No “we’ll email it.”
- Plan your follow-up. Don’t assume your local doctor will know what to do. Book a post-travel appointment before you leave. Bring your discharge papers and pill photos.
What Happens When You Get Home
Most medical tourists don’t realize their biggest risk comes after they land.
Studies show 26% of medical tourists face follow-up care issues. A huge chunk of those are medication-related:
- You can’t refill your painkiller because it’s not approved here.
- Your blood thinner is different, and your doctor won’t prescribe it without knowing the source.
- You’re given supplements or herbal remedies abroad that clash with your heart medication.
Some patients end up in emergency rooms because they didn’t tell their doctor about the foreign meds. Others stop taking their drugs because they can’t get them-and then suffer complications.
Telemedicine and digital health records are starting to help. Some clinics now share records directly with overseas doctors. But that’s still the exception-not the rule.
Wellness Tourism Is a Hidden Danger Zone
More people are combining medical procedures with “wellness retreats”-yoga, detoxes, IV vitamin drips, stem cell therapies.
Here’s the problem: These aren’t regulated like real medicine. A clinic in Bali might offer “anti-aging injections” made from unapproved substances. A clinic in Mexico might sell “stem cell therapy” using cells that haven’t been tested for safety.
These aren’t just scams. They’re medical risks. Some of these treatments interact dangerously with prescription drugs. Others cause infections, allergic reactions, or long-term damage.
If it sounds too good to be true-like “cure your diabetes in 3 days with a shot”-it is. And the pills or shots you’re given? They’re not on any safety list.
Who’s Doing It Right?
Some countries are stepping up. South Korea now uses AI to personalize cancer drug regimens based on your DNA. That’s advanced. But even there, if you’re not a local, you might not get the same access to follow-up care.
Thailand has over 100 JCI-accredited hospitals. Many of them work with international insurers and have clear medication protocols. But again-this doesn’t mean every drug they use is approved in your country.
The safest bet? Choose a destination with strong regulatory alignment. Turkey, for example, follows EU standards. That means many of their drugs are the same as those in Australia or the UK. Mexico’s top medical tourism centers often use U.S.-approved drugs. But always verify.
Final Warning: The Industry Isn’t Fixing This
The medical tourism market is projected to hit over $700 billion by 2033. Billions are being made. But there’s no global agency tracking medication safety for travelers. No watchdog. No mandatory reporting.
Doctors in your home country aren’t trained to handle foreign prescriptions. Pharmacists don’t have databases for drugs from Cambodia or Georgia. Insurance companies won’t cover complications from treatments abroad.
So the burden falls on you.
You’re not just buying a procedure. You’re buying a chain of medications-each one a potential risk. Don’t skip the steps. Don’t assume it’s safe because it’s cheap. Your health isn’t a bargain bin item.
What to Do If Something Goes Wrong
If you experience side effects, allergic reactions, or notice your medication doesn’t match what was described:
- Stop taking it immediately.
- Take a photo of the pill and packaging.
- Go to your local ER or doctor with your discharge papers and photos.
- Report it to your country’s health authority (e.g., TGA in Australia).
Don’t wait. Don’t hope it goes away. Medication errors can escalate fast.
Vicki Yuan
January 4, 2026 AT 17:42I got a knee replacement in Bangkok last year, and I did every single thing the article said. I took photos of every pill, wrote down batch numbers, and emailed my pharmacist back home before I left. They actually had a database match for the generic name. No drama. No ER visits. Just a healthy knee and peace of mind.
Uzoamaka Nwankpa
January 5, 2026 AT 21:54People who travel for medical care are either desperate or foolish. There is no middle ground. You think you're saving money, but you're gambling with your life, and you don't even know the rules of the game.
jigisha Patel
January 6, 2026 AT 01:50While the article correctly identifies the risks associated with substandard pharmaceuticals in low-regulation jurisdictions, it fails to contextualize the prevalence of counterfeit medications within domestic supply chains. A 2022 FDA report indicated that approximately 3% of medications dispensed in the United States were misbranded or adulterated-comparable to rates in some Southeast Asian nations. The narrative of ‘foreign danger’ is misleading and distracts from systemic failures in local healthcare infrastructure.
Jason Stafford
January 6, 2026 AT 13:12Did you know the FDA is in on it? They let these drugs in because Big Pharma wants you dependent on their overpriced pills. The moment you step off the plane with that ‘unapproved’ medication, they’re already tracking your DNA through your pharmacy records. They want you scared of cheap meds so you keep paying $800 for a bottle of ibuprofen. This isn’t about safety-it’s about control.
Michael Rudge
January 7, 2026 AT 12:39Oh wow, someone wrote a 2,000-word essay on how not to be an idiot? Groundbreaking. I’m sure the 14 million people who’ve done this without dying are just too dumb to notice the ‘life-or-death’ stakes you so eloquently pointed out. Maybe next time, don’t write like you’re trying to scare people into buying your ebook.
Cassie Tynan
January 9, 2026 AT 11:02It’s funny how we treat medicine like it’s a luxury product you can just ‘shop around’ for. We don’t do that with our cars or our homes. Why do we think our bodies are any different? Maybe the real problem isn’t the foreign pharmacy-it’s that we’ve turned healthcare into a market, not a right.
Catherine HARDY
January 10, 2026 AT 02:17I read this article and immediately thought: what if the pills I took in Mexico were laced with fentanyl? I didn’t even think to check the batch number. Now I’m terrified every time I take a painkiller. I’m not even sure I can trust my own medicine anymore. I think I’m going to stop taking all of it until I can prove it’s safe.
bob bob
January 11, 2026 AT 19:50My cousin went to India for a heart stent. Got home, couldn’t refill the meds. Called his doc, who said ‘I’ve never seen that brand.’ So he called the hospital in Mumbai, got the generic name, and his pharmacist found a US equivalent. Took 48 hours. He’s fine now. Just talk to people. Don’t panic.
Chris Cantey
January 13, 2026 AT 04:06There’s a deeper truth here: we’ve outsourced our vulnerability. We don’t trust our own systems, so we go abroad for cheaper care-but we never question why our own system failed us in the first place. The medication isn’t the enemy. The system that makes you choose between bankruptcy and a foreign pill is.
Abhishek Mondal
January 13, 2026 AT 14:04Let me be clear: the article’s recommendations are superficial. You mention ‘generic names’-but have you considered the pharmacokinetic variability between ethnic populations? A dose calibrated for a Caucasian male may be toxic for an Indian female with CYP2C19 polymorphism. You’re advocating for surface-level due diligence while ignoring the genetic reality of pharmacogenomics. This is not safety-it’s pseudosafety.
Oluwapelumi Yakubu
January 13, 2026 AT 20:34My brother went to Turkey for a dental implant and came back with a smile and a new life. He asked for the drug names, took pictures, and even sent the bottle to his dentist here in Lagos. They checked it against the EU database-everything was legit. The real secret? Don’t be lazy. Ask questions. Be curious. And don’t let fear stop you from living.
Terri Gladden
January 14, 2026 AT 15:01i went to mexico for a tummy tuck and they gave me this blue pill that looked like a skywalker from star wars and now im paranoid every time i sneeze and i think my liver is plotting against me help
Jennifer Glass
January 16, 2026 AT 09:36I think the most important thing the article missed is this: when you go abroad for care, you’re not just a patient-you’re a traveler in a foreign medical culture. Just like you learn the language and customs, you need to learn how the pharmacy system works. It’s not about fear. It’s about adaptation.
en Max
January 18, 2026 AT 04:43Based upon the empirical data presented in this exposition, it is imperative to acknowledge that the absence of harmonized pharmacovigilance frameworks across international jurisdictions constitutes a critical systemic vulnerability. The proliferation of non-standardized pharmaceutical supply chains, coupled with the non-interoperability of electronic health records, engenders a non-trivial risk profile for transnational medical tourists. Mitigation strategies must therefore incorporate: (1) pre-travel pharmacogenomic screening; (2) blockchain-verified drug traceability; and (3) mandatory bilateral regulatory reciprocity agreements between source and destination nations. Without these, the current paradigm is unsustainable.