Exercise and Chronic Heart Failure: Staying Active Safely
 Oct, 6 2025
Oct, 6 2025
Heart Failure Exercise Planner
Exercise Safety Tips
- Use a wearable heart-rate monitor to stay within target zones
- Practice the Talk Test - you should be able to speak in short sentences
- Stop immediately if you experience chest pain, dizziness, or shortness of breath
- Stay hydrated and monitor your weight daily
- Follow your prescribed medication schedule
Living with chronic heart failure is a daily juggling act. Your heart struggles to pump enough blood, so you might wonder: can I still move, jog, or lift light weights without risking a setback? The answer is yes - but only when you follow a plan that respects your heart’s limits. This guide shows exactly how to stay active, avoid danger, and reap the heart‑boosting benefits of exercise.
Key Takeaways
- Exercise improves strength, mood, and survival rates for people with chronic heart failure.
- Start with a medical clearance and a simple symptom checklist.
- Aerobic, resistance, flexibility, and balance work together for a well‑rounded routine.
- Use a wearable heart‑rate monitor and the Talk Test to stay within safe intensity zones.
- A 3‑day‑a‑week plan of 20‑30 minutes each session is enough to see progress.
What Is Chronic Heart Failure?
Chronic heart failure is a condition where the heart cannot pump blood efficiently enough to meet the body’s needs. It affects roughly 2% of adults over 65 in Australia, and the prevalence rises with age. Two key clinical markers help doctors describe the disease:
- Ejection fraction measures the percentage of blood pumped out of the left ventricle with each beat, usually expressed as a value between 30% and 55%. Lower numbers indicate more severe systolic dysfunction.
- NYHA classification categorises symptoms from Class I (no limitation) to Class IV (symptoms at rest). Knowing your class guides exercise intensity.
The condition doesn’t mean you must stay glued to the couch; it means you need a smart, monitored approach.
Why Exercise Matters
Exercise is any bodily activity that raises heart rate and uses muscles offers more than calorie burn. In chronic heart failure, regular activity:
- Improves cardiac output by enhancing muscle efficiency.
- Reduces hospital admissions by up to 30% (study of 2,500 patients, 2023).
- Lowers blood pressure, improves cholesterol, and helps control weight.
- Boosts mental health - depression rates drop by 40% after six months of structured activity.
But the benefits only appear when you stay within safe zones, which is why a clear plan matters.
Getting Started Safely
Before you lace up sneakers, follow these three steps:
- Medical clearance. Ask your cardiologist for a written ok, mentioning your NYHA class and current medications (beta‑blockers, ACE inhibitors, etc.).
- Symptom checklist. Record any chest pain, dizziness, unusual shortness of breath, or swelling that worsens during activity. If any appear, stop and call your doctor.
- Baseline measurements. Note resting heart rate, blood pressure, and perceived exertion using the Talk Test (you should be able to speak in short sentences).
With clearance, you can design a program that progresses slowly.
Choosing the Right Types of Exercise
Think of exercise as a toolbox. Each tool targets a specific need.
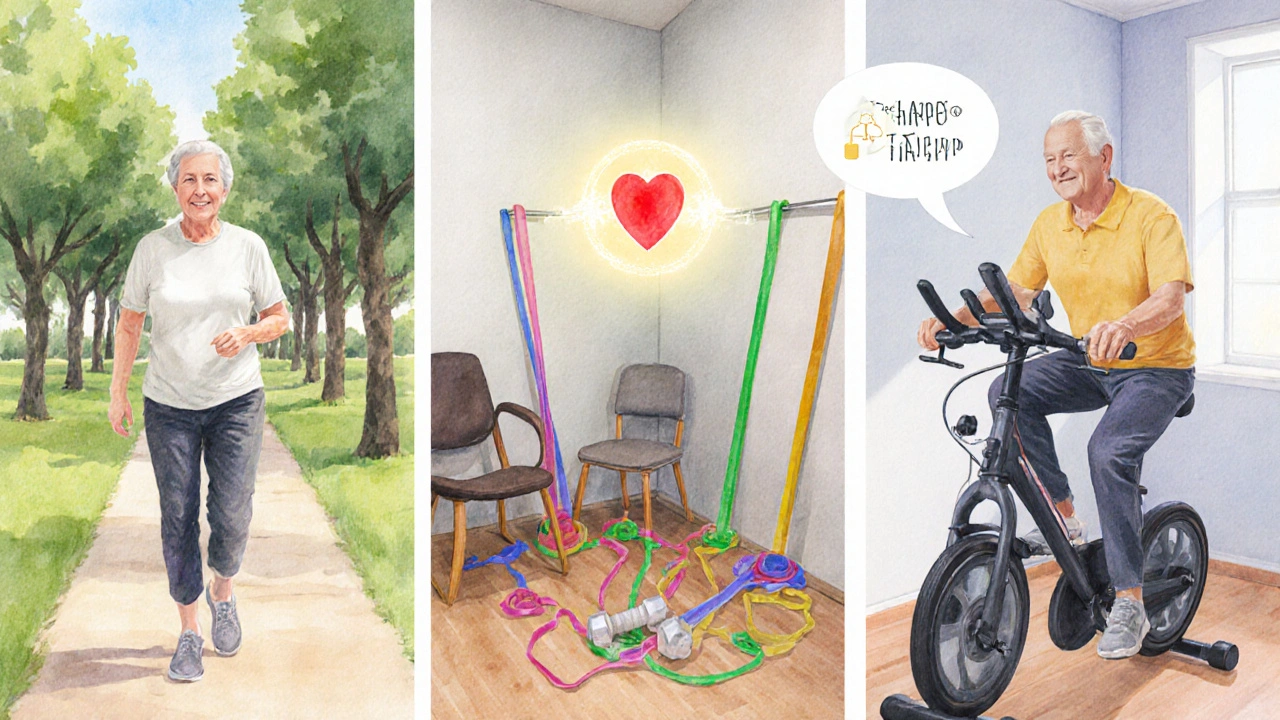
Aerobic Exercise
Aerobic exercise includes activities that keep the heart moving for extended periods, like walking, cycling, or swimming. It builds endurance and improves oxygen delivery.
Resistance Training
Resistance training uses weights, bands, or body weight to strengthen muscles. Stronger muscles need less oxygen, easing the heart’s workload.
Flexibility and Balance
Gentle stretching and balance drills reduce fall risk, a common concern for older adults with heart failure.
Monitoring Your Effort
The safest way to know you’re in the right zone is a wearable heart‑rate monitor. Look for devices that show real‑time beats‑per‑minute and allow you to set alerts for a target range (usually 50‑70% of your maximum heart rate, calculated as 220 minus age). Pair this with the Talk Test: if you can hold a conversation without gasping, you’re likely in the correct moderate zone.

Sample Weekly Plan (20‑30min Sessions)
| Aspect | Low‑Impact (e.g., walking) | Moderate‑Impact (e.g., brisk cycling) |
|---|---|---|
| Heart‑rate range | 50‑60% of max | 60‑70% of max |
| Joint stress | Minimal | Moderate |
| Typical duration | 20min | 30min |
| Calorie burn | ~120kcal | ~200kcal |
Here’s how a beginner might schedule the week:
- Monday - 20min walk (low‑impact, heart rate 55% of max, end with 5‑minute cool‑down stretch).
- Wednesday - 15min resistance circuit (body‑weight squats, wall push‑ups, seated rows with resistance band; 2sets of 10 reps each).
- Friday - 25min stationary bike (moderate‑impact, keep heart rate in 65% zone, finish with 5min slow pedal).
- Optional Saturday - 10min balance drills (single‑leg stands, heel‑to‑toe walk).
Increase either duration or intensity by about 10% each week, never jumping more than two levels at a time.
Common Pitfalls and How to Avoid Them
- Skipping warm‑up. Jumping straight into activity spikes blood pressure. Always spend 5minutes on low‑intensity movement.
- Ignoring medication timing. Beta‑blockers lower heart rate, so you may need a slightly higher perceived effort to hit your target zone.
- Over‑relying on the watch. If the monitor beeps, pause and assess symptoms first - numbers can’t replace how you feel.
- Doing too much, too fast. Adhering to the 10% rule prevents dangerous spikes in demand on the heart.
Next Steps & Troubleshooting
If you feel unusually tired after a session, check your fluid intake and electrolytes; dehydration can mimic heart‑failure symptoms. Persistent swelling or shortness of breath deserves a call to your cardiology clinic. For those who struggle with motivation, consider joining a local cardiac rehabilitation program that offers supervised exercise, education, and peer support. Studies show participants have 25% lower readmission rates.
Frequently Asked Questions
Can I do high‑intensity interval training (HIIT) with chronic heart failure?
HIIT can be safe for select patients in NYHA Class I‑II who have physician clearance, but it should start with very short bursts (10‑15 seconds) and long recovery periods. Most experts recommend sticking to moderate‑intensity continuous exercise for the majority of patients.
How often should I check my weight to monitor fluid retention?
Weigh yourself daily, preferably in the morning after using the bathroom and before breakfast. A gain of more than 2kg (4.4lb) over three days warrants a call to your doctor.
Is swimming better than walking for heart failure patients?
Both are excellent low‑impact options. Swimming adds resistance from water, which can boost muscle strength without stressing joints. Choose whichever you enjoy more, as adherence is the key driver of benefit.
What heart‑rate range should I aim for during exercise?
Target 50‑70% of your age‑predicted maximum (220-age). For a 65‑year‑old, that’s roughly 77‑108bpm. Adjust down if you’re on beta‑blockers or feel breathless.
Can I exercise if I have an implanted cardioverter‑defibrillator (ICD)?
Yes, most patients can continue moderate activity after a healing period of 4‑6 weeks post‑implant. Use a heart‑rate monitor and avoid contact sports that might damage the device.
Craig Mascarenhas
October 6, 2025 AT 16:06It seems the exercise guidelines are a smokescreen crafted by big pharma to keep heart failure patients reliant on costly drugs.
aarsha jayan
October 13, 2025 AT 14:50What a vibrant roadmap for staying active! Your plan combines gentle movement with safety, making it feel like a friendly dance that anyone can join.
Rita Joseph
October 13, 2025 AT 14:55First and foremost, congratulations on taking the step to understand how exercise can coexist with chronic heart failure.
The evidence base from recent cardiology trials shows that even low‑impact activity can improve ejection fraction over time.
When you begin, focus on the Talk Test – if you can hold a brief conversation without gasping, you’re likely in the safe zone.
Remember to warm up for at least five minutes; this gradual ramp up prevents sudden spikes in blood pressure.
Wear a reliable heart‑rate monitor and set alerts for the 50‑70 % of your age‑predicted maximum.
If you’re on beta‑blockers, your resting heart rate may be lower, so rely more on perceived exertion than raw numbers.
Hydration is essential – a modest 1‑2 L per day helps maintain plasma volume and reduces the risk of orthostatic dizziness.
Daily weight checks are a simple yet powerful tool; a gain of more than 2 kg over three days should trigger a call to your clinician.
Incorporate resistance training twice a week using light bands or body weight; stronger peripheral muscles lower the heart’s workload during daily tasks.
Balance drills, such as single‑leg stands, can dramatically cut fall risk, a common concern in this population.
Adopt the 10 % rule: increase either duration or intensity by no more than ten percent each week to avoid over‑taxing the heart.
Schedule rest days; they’re not a sign of weakness but a physiological necessity for cardiac remodeling.
Keep a log of symptoms – chest discomfort, undue shortness of breath, or swelling – and share it with your care team promptly.
If an implanted cardioverter‑defibrillator is present, avoid high‑impact contact sports for at least six weeks post‑implant and always inform your provider before starting a new regimen.
Finally, consider joining a supervised cardiac rehabilitation program; peer support and professional oversight boost adherence and outcomes.
Stay consistent, listen to your body, and celebrate each incremental gain; your heart will thank you.
abhi sharma
October 13, 2025 AT 14:59Nice plan.
mas aly
October 13, 2025 AT 15:03I appreciate the thorough overview, especially the emphasis on gradual intensity increments and the practical advice on using the Talk Test.
Abhishek Vora
October 13, 2025 AT 15:07Allow me to elucidate: the physiological premise is unequivocal-incremental aerobic load augments myocardial efficiency while preserving hemodynamic stability.
maurice screti
October 13, 2025 AT 15:11Honestly, when one scrutinizes the quintessence of cardiovascular conditioning, the interplay between preload augmentation and afterload reduction becomes an art form, and this guide captures that nuance with a commendable flair.
Abigail Adams
October 13, 2025 AT 15:16While your prose is undeniably ornate, the practical takeaway remains that patients should prioritize safety over stylistic embellishment.
Belle Koschier
October 13, 2025 AT 15:20Great job highlighting balance drills; they’re essential for preventing falls and building confidence in daily activities.
Allison Song
October 13, 2025 AT 15:24From a broader perspective, incorporating movement into one’s routine reflects the ancient principle that the body is a vessel for the soul’s journey.
Joseph Bowman
October 13, 2025 AT 15:28Indeed, the subtle forces that steer modern healthcare often overlook such holistic wisdom, but we can reclaim agency through mindful exercise.
Singh Bhinder
October 13, 2025 AT 15:32It's worth noting that beta‑blockers can blunt heart‑rate response, so adjusting target zones accordingly is crucial.
Kelly Diglio
October 13, 2025 AT 15:37Excellent reminder to weigh daily; a sudden increase of >2 kg over 72 hours warrants immediate medical consultation! 😊
Carmelita Smith
October 13, 2025 AT 15:41Love the weekly schedule-keeps things simple! 👍
Liam Davis
October 13, 2025 AT 15:45Indeed, structured consistency minimizes the risk of overexertion while fostering progressive adaptation. 🚀
Arlene January
October 13, 2025 AT 15:49Let’s keep the momentum going-every step counts, no matter how tiny!
Kaitlyn Duran
October 13, 2025 AT 15:53Adding a short warm‑up jog before the main session can prime muscles and improve circulation.
Terri DeLuca-MacMahon
October 13, 2025 AT 15:58Stay hydrated, keep smiling, and remember: your heart is stronger than you think! 🌟💪
gary kennemer
October 13, 2025 AT 16:02Reflecting on the interplay between effort and recovery, one finds that balance is the true hallmark of sustainable health.
Payton Haynes
October 13, 2025 AT 16:06The devices that monitor our vitals could be feeding data to unseen algorithms that influence treatment plans.