Vaginal Surgery: What It Is, How to Prepare, and Recovery Basics
If you or someone you know is facing a vaginal surgery, the first thing that comes to mind is often anxiety. You might wonder what the operation involves, how long it will take, and what life looks like afterward. This guide breaks down the most common procedures, gives clear steps for getting ready, and offers practical tips to help you heal faster.
Common Types of Vaginal Surgery
There are several reasons a doctor may suggest a vaginal approach. The most frequent surgeries include:
- Vaginal hysterectomy – removal of the uterus through the vagina, often used for fibroids or heavy bleeding.
- Sacrocolpopexy (or sacrospinous ligament fixation) – a repair to support a prolapsed organ like the bladder or rectum.
- Labiaplasty – reshaping of the labia for comfort or cosmetic reasons.
- Perineoplasty – reconstruction of the tissue between the vagina and anus after childbirth tears.
- Vaginal sling procedures – support for stress urinary incontinence using a mesh or tape.
All these surgeries share a common goal: fix an issue while keeping incisions hidden inside the body. That usually means less pain, quicker recovery, and no external scar.
Preparing for Your Procedure
Good preparation makes surgery smoother. Start by talking openly with your surgeon about any medicines you take – blood thinners, supplements, or even over‑the‑counter pain relievers can affect bleeding. Your doctor will likely ask you to stop certain drugs a week before the operation.
Next, arrange a support system. Have someone drive you home and stay for at least 24 hours. Stock up on easy‑to‑eat foods like yogurt, soup, or smoothies because you’ll want soft meals while your stitches heal.
Don’t forget to plan for hygiene. You’ll be instructed to use a peri bottle (a small squirt bottle) with warm water after bathroom trips. Having this ready before you leave the hospital cuts down on discomfort later.
What Happens After Surgery
Most vaginal surgeries are done as day‑cases or require an overnight stay. You’ll wake up with a catheter in place to keep the bladder empty while swelling goes down. The catheter usually comes out within 24 hours, and you can start gentle walking right away – movement helps prevent blood clots.
Stitches inside the vagina dissolve on their own, so you won’t need a follow‑up visit just for removal. However, schedule a post‑op appointment to let your surgeon check that everything is healing correctly.
Avoid heavy lifting, straining, or intense exercise for at least four weeks. Light activities like short walks are fine and actually help circulation. If you notice increasing pain, fever, or unusual discharge, call your doctor right away.
Tips to Speed Up Healing
- Stay hydrated: plenty of water helps tissue repair.
- Eat protein‑rich foods: eggs, lean meat, beans give your body the building blocks for healing.
- Follow pelvic floor exercises only when your surgeon says it’s safe – they can improve strength but doing them too early may stress stitches.
- Keep the area clean: use the peri bottle after each bathroom visit and pat dry gently.
- Rest with pillows under your hips while sitting to reduce pressure on the surgical site.
Every woman’s recovery timeline is a bit different, but most people feel back to normal activities within six weeks. Patience and following your doctor’s instructions are the best tools you have.
If you’re looking for more details about specific procedures or want to read personal stories, check out our other articles on the site. They cover everything from choosing a surgeon to managing pain without strong opioids.
Remember, vaginal surgery is a routine solution that can dramatically improve quality of life. With the right prep and after‑care, you’ll be back to your daily routine sooner than you think.
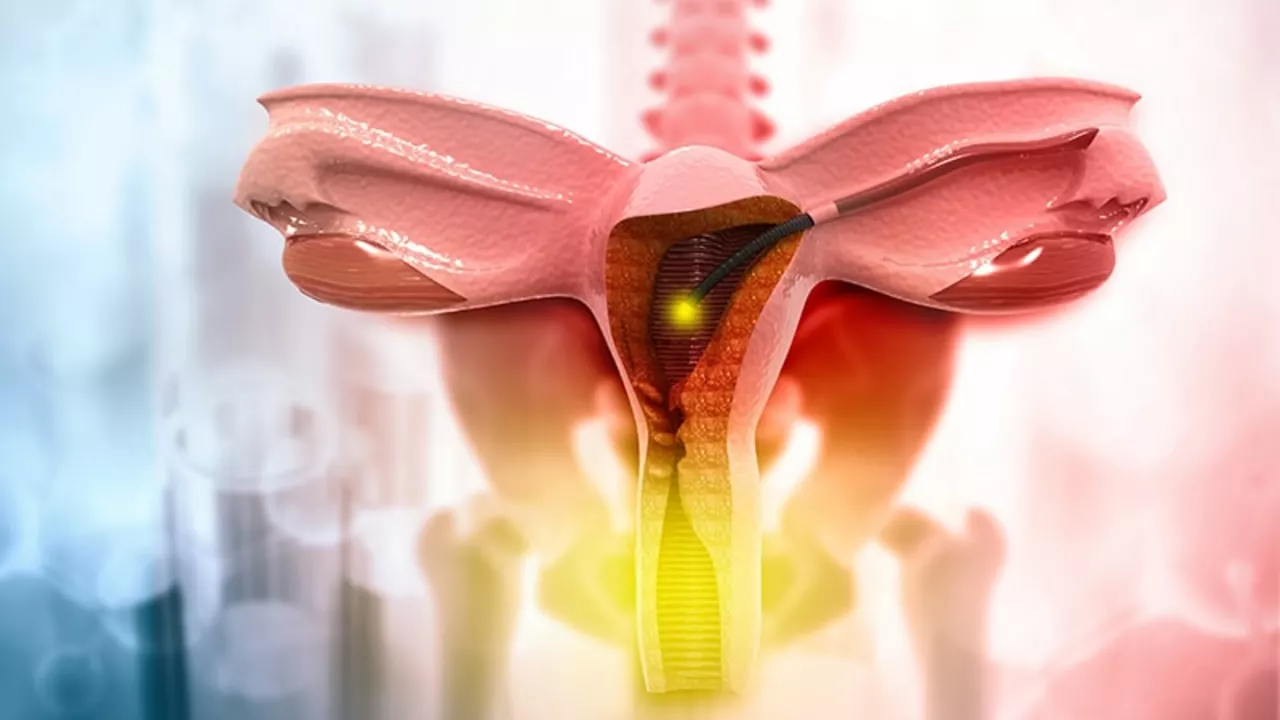
How Vaginal Surgery Treats Pelvic Organ Prolapse - Benefits, Risks, and Options
Explore how vaginal surgery treats pelvic organ prolapse, from native‑tissue repairs to mesh and apical suspensions, with risks, recovery tips, and future trends.
Addressing the misconceptions about surgery on vagina
In my latest post, I've tried to clear up some common misconceptions about vaginal surgery. Firstly, I tackled the myth that such procedures are purely cosmetic, highlighting their valuable role in addressing medical issues like incontinence or prolapse. I also dispelled the notion that recovery is overly lengthy and painful - with modern techniques, it's often quicker and less discomforting than many believe. Additionally, I emphasized that vaginal surgery does not necessarily diminish sexual pleasure; in fact, it can enhance it in several cases. Lastly, I explained that these surgeries are not exclusively for older women, but they may be beneficial for younger women too based on their personal health circumstances.