Pelvic Organ Prolapse: Causes, Symptoms, and Treatment Options
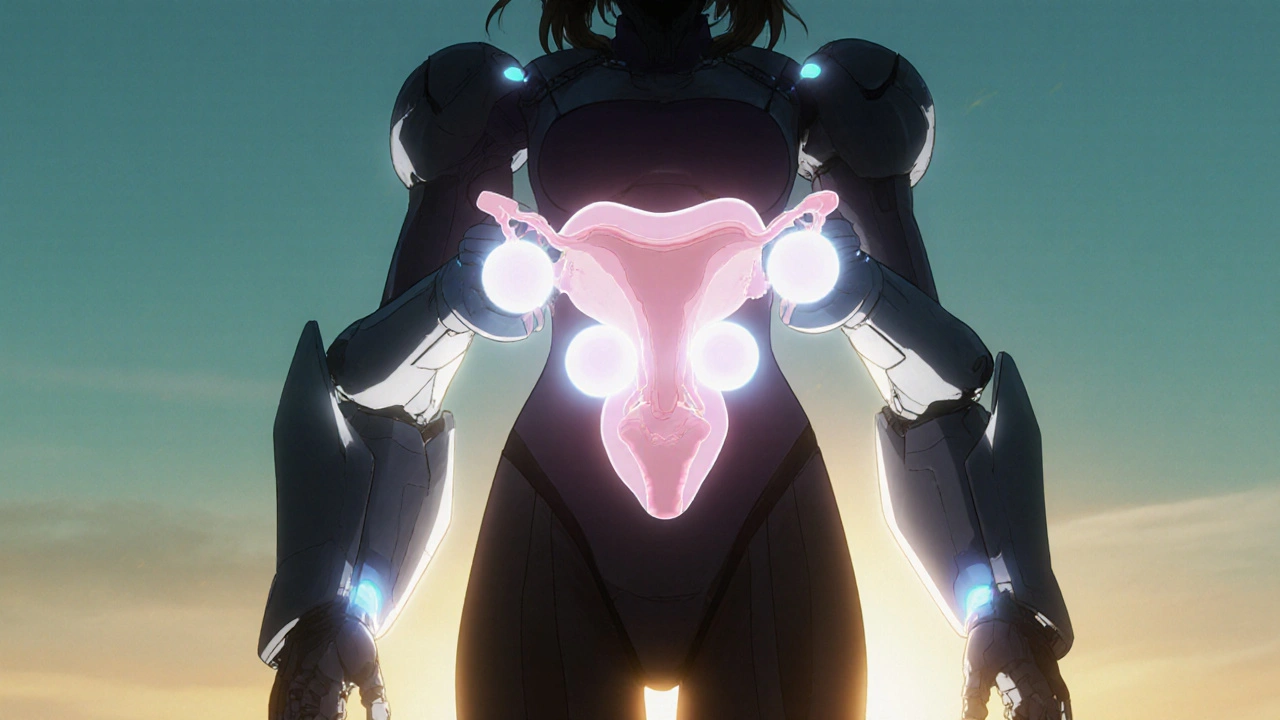
When the muscles and tissues holding your pelvic organs in place weaken, those organs—like the bladder, uterus, or rectum—can drop down and press into or out of the vagina. This is called pelvic organ prolapse, a condition where pelvic organs descend from their normal position due to weakened support structures. It’s not rare, and it’s not something to be ashamed of. Many women experience it after childbirth, menopause, or years of heavy lifting. Also known as pelvic floor descent, the downward shift of pelvic organs due to loss of muscular support, it affects nearly half of women who’ve given birth, and the risk goes up with age.
What causes it? Think of your pelvic floor like a hammock. If it’s stretched too much—by pregnancy, chronic coughing, obesity, or even long-term constipation—it loses its tension. The result? Your bladder might bulge into the vagina (cystocele), your uterus might drop (uterine prolapse), or your rectum might push outward (rectocele). You might feel pressure, notice a bulge, have trouble peeing or pooping, or feel like something’s falling out. Some women don’t feel anything until it’s advanced. And yes, it can happen even if you’ve never had kids—aging, genetics, and long-term physical strain play big roles.
It’s not just about surgery. Many women find relief with pelvic floor therapy, targeted exercises and manual techniques to strengthen the muscles supporting pelvic organs. Kegels, biofeedback, and specialized physical therapy can make a real difference. For others, a pessary—a small device inserted into the vagina to hold organs in place—works well without surgery. If symptoms are severe or interfere with daily life, prolapse surgery, procedures designed to restore pelvic organ position through repair or support is an option. There are different types, from minimally invasive to reconstructive, and recovery varies.
What you’ll find in the posts below isn’t a textbook. It’s real talk about what works. You’ll see comparisons of medications that help with related symptoms like urinary incontinence, how certain drugs might affect pelvic floor health, and what lifestyle changes actually make a difference. Some posts dig into how hormone changes after menopause impact pelvic support. Others look at how common treatments for other conditions—like long-term use of acid blockers or diuretics—might quietly worsen pelvic pressure. You won’t find fluff. Just clear, practical info from people who’ve been there and experts who’ve studied it.
How Vaginal Surgery Treats Pelvic Organ Prolapse - Benefits, Risks, and Options
Explore how vaginal surgery treats pelvic organ prolapse, from native‑tissue repairs to mesh and apical suspensions, with risks, recovery tips, and future trends.