Quinolone Antibiotics and Corticosteroids: The Real Risk of Tendon Rupture
 Feb, 11 2026
Feb, 11 2026
When you take an antibiotic like ciprofloxacin for a stubborn urinary infection, you probably don’t think about your tendons. But if you’re over 60 and also taking a steroid like prednisone for arthritis or asthma, you could be putting yourself at serious risk - not for an allergic reaction or stomach upset, but for a tendon rupture. This isn’t a rare side effect you read about in fine print. It’s a well-documented, preventable injury that sends people to the ER, often with no warning.
How a Common Antibiotic Can Tear Your Tendon
Quinolone antibiotics - especially fluoroquinolones like ciprofloxacin, levofloxacin, and norfloxacin - were once among the most prescribed drugs in the world. They work great against tough infections: pneumonia, complicated UTIs, even some kinds of food poisoning. But around the early 2000s, doctors started noticing a pattern. Patients on these drugs, especially older adults, were showing up with sudden, excruciating pain in their heels - often while walking or climbing stairs. No trauma. No fall. Just a popping sound, then an inability to push off the foot. That’s Achilles tendon rupture. And it’s not a coincidence. A 2000 study in JAMA Internal Medicine found that fluoroquinolones increase the risk of Achilles tendon rupture by more than four times. The tendon doesn’t just weaken - it can tear after just one dose. Some cases happened within days. Others popped up weeks after the antibiotic was stopped. The mechanism isn’t fully understood, but research points to direct damage to collagen, the main structural protein in tendons. Fluoroquinolones seem to interfere with how tendon cells (tenocytes) repair themselves. They may trigger enzymes that break down collagen faster than the body can rebuild it. The result? A tendon that looks normal on the outside but is crumbling from within.The Perfect Storm: When Steroids Make Things Worse
Here’s where it gets dangerous. If you’re already taking corticosteroids - whether it’s a pill for inflammation, an injection for joint pain, or an inhaler for COPD - your risk skyrockets. A landmark study using data from the UK’s General Practice Research Database found that people taking both a fluoroquinolone and a corticosteroid had a 46-fold higher risk of tendon rupture than those taking neither. Why? Corticosteroids suppress inflammation and healing. They also directly weaken connective tissue. So while the antibiotic is silently damaging the tendon’s structure, the steroid is stopping the body’s repair efforts. It’s like drilling holes in a rope while someone cuts the strands with a knife. One alone might not break it. Together? It snaps. This isn’t theoretical. In New Zealand, between 2007 and 2012, 53 cases of tendon injury linked to fluoroquinolones were reported to their national monitoring system. Ciprofloxacin was behind 68% of them. Norfloxacin was next. And in nearly 90% of those cases, the Achilles tendon was the one that failed.Who’s Most at Risk?
Not everyone who takes these drugs will rupture a tendon. But certain people are in the danger zone:- Age 60+: Risk doubles for tendon disorders and triples for rupture compared to younger adults.
- On corticosteroids: Oral, injected, or inhaled - all count. Even low-dose daily prednisone raises the risk.
- Have kidney problems: Especially if your eGFR is below 30. Fluoroquinolones are cleared by the kidneys. Poor function means the drug builds up, increasing exposure.
- Diabetic: High blood sugar damages collagen and impairs healing.
- History of tendon injury: If you’ve had a prior rupture or tendon surgery, your tissue is already vulnerable.
- Organ transplant recipients: These patients often take long-term steroids and are frequently treated with antibiotics.
What Does a Tendon Rupture Feel Like?
Most people don’t notice tendinitis - the warning sign - until it’s too late. But if you do, here’s what to watch for:- Sudden, sharp pain in the back of the ankle, shoulder, or wrist during normal movement
- Swelling or warmth around the tendon
- A feeling of “tightness” or stiffness that doesn’t go away
- Difficulty walking, especially pushing off with the foot
- A loud pop or snap (often described as feeling like someone kicked you in the heel)
What Happens After a Rupture?
This isn’t a sprain. It’s a complete tear. Recovery takes 6 to 12 months. Most people need surgery. Even with surgery, you’ll be in a cast or boot for weeks, then months of physical therapy. Many never fully regain their previous strength or mobility. A 2003 study estimated that 2% to 6% of all Achilles ruptures in people over 60 are directly caused by fluoroquinolones. That’s not a small number. In a city like Melbourne, with a large aging population, that’s dozens of preventable injuries every year. And it’s not just the Achilles. While 89% of cases involve the heel tendon, shoulder tendons (rotator cuff) and wrist tendons (like the biceps) are also at risk. One patient might rupture their Achilles while walking the dog. Another might tear their shoulder tendon lifting groceries. Both were on ciprofloxacin. Both were on steroids.Doctors Know This. So Why Are These Drugs Still Prescribed?
Fluoroquinolones are powerful. They work against bacteria that other antibiotics can’t touch. For a life-threatening infection - like sepsis or a complicated kidney infection - the benefits still outweigh the risks. But here’s the problem: they’re often prescribed for things they shouldn’t be. A sinus infection? A mild UTI? Bronchitis? These are usually viral or can be treated with safer options. Yet fluoroquinolones are still handed out like candy. In 2013, the U.S. FDA added a “black box” warning - their strongest alert - to all systemic fluoroquinolones. It said: Don’t use these for routine infections when safer alternatives exist. The European Medicines Agency followed suit. New Zealand’s Medsafe issued a prescriber alert in 2012. But prescribing habits change slowly. A 2025 review in the Australian Journal of General Practice found that 17% of fluoroquinolone prescriptions in patients over 60 were for conditions with clear alternatives - like amoxicillin or nitrofurantoin.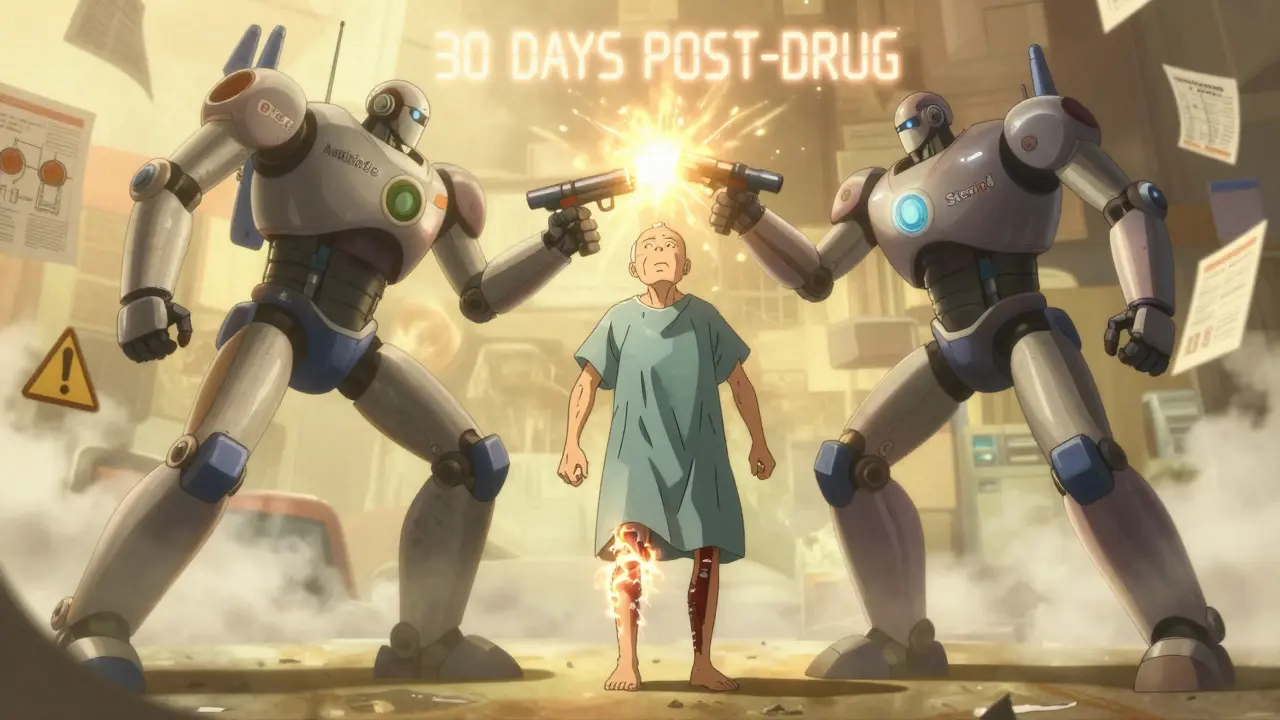
What Should You Do?
If you’re over 60, on steroids, and your doctor suggests a fluoroquinolone:- Ask: “Is there another antibiotic that works just as well?”
- Ask: “What’s the risk of tendon rupture if I take this?”
- Ask: “Can we try a shorter course?”
What’s Being Done Now?
Regulators aren’t sitting still. The FDA’s Adverse Event Reporting System (FAERS) still flags tendon rupture as one of the top concerns with fluoroquinolones. Researchers are now looking at blood biomarkers - proteins that might signal early tendon damage - to help identify high-risk patients before they get hurt. Some labs are testing next-generation quinolones that don’t bind as tightly to human collagen. But those are years away. For now, the message is simple: Don’t take fluoroquinolones unless you absolutely need them - especially if you’re on steroids.Final Thought
Antibiotics save lives. But they’re not harmless. The risk of tendon rupture with fluoroquinolones and corticosteroids is rare - about 0.1% to 0.4% of users - but devastating. It’s not something you recover from in a week. It’s a life-altering injury that can leave you dependent on crutches, walkers, or surgery for over a year. Your doctor isn’t trying to harm you. But they might not know the full risk. Or they might assume you’re fine because you’re “otherwise healthy.” You need to speak up. Ask the questions. Push for alternatives. Because your tendon isn’t just tissue - it’s what lets you walk, climb stairs, play with your grandkids, or just get out of bed without help.Can fluoroquinolones cause tendon rupture even after stopping the drug?
Yes. Up to 50% of tendon ruptures linked to fluoroquinolones occur after the patient has finished the course. The damage to collagen can take weeks to manifest, and the tendon remains vulnerable for months after the drug is cleared from the body. This is why doctors warn patients to stay alert for pain or swelling even after finishing the antibiotic.
Which fluoroquinolone has the highest risk of tendon rupture?
Ciprofloxacin is the most commonly reported fluoroquinolone associated with tendon rupture, accounting for nearly 70% of cases in multiple international databases. Norfloxacin is second, followed by levofloxacin. All fluoroquinolones carry the risk, but ciprofloxacin has the strongest association in real-world data.
Are topical steroids as risky as oral steroids when combined with fluoroquinolones?
Topical steroids - like creams or ointments - are unlikely to raise the risk significantly because they don’t enter the bloodstream in large amounts. However, injected steroids (like cortisone shots) and inhaled steroids (for asthma or COPD) can. If you’ve had a steroid injection in your shoulder or ankle recently, that counts as a risk factor. Always tell your doctor about all steroid use, even if it’s not oral.
Is there a safe alternative to fluoroquinolones for a UTI?
Yes. For uncomplicated urinary tract infections, nitrofurantoin and trimethoprim-sulfamethoxazole are first-line options and don’t carry tendon rupture risk. Amoxicillin-clavulanate is another safe choice. Fluoroquinolones should only be used if these fail, the infection is severe, or the bacteria are resistant. Always ask: "Is this the best option for me?"
What should I do if I feel tendon pain while on a fluoroquinolone?
Stop taking the antibiotic immediately. Avoid putting stress on the affected area - no running, jumping, or heavy lifting. Call your doctor right away. An ultrasound can confirm whether there’s inflammation or partial tearing. Early action can prevent a full rupture. Do not wait to see if it "goes away."
Jonathan Noe
February 12, 2026 AT 00:16Pat Mun
February 13, 2026 AT 16:45Annie Joyce
February 15, 2026 AT 14:17Sonja Stoces
February 16, 2026 AT 18:13Jim Johnson
February 17, 2026 AT 16:29Luke Trouten
February 17, 2026 AT 23:41Kristin Jarecki
February 18, 2026 AT 02:25Suzette Smith
February 19, 2026 AT 05:06Gloria Ricky
February 19, 2026 AT 13:12Craig Staszak
February 21, 2026 AT 07:29Skilken Awe
February 21, 2026 AT 21:48Vamsi Krishna
February 23, 2026 AT 19:00Jason Pascoe
February 24, 2026 AT 15:15alex clo
February 25, 2026 AT 23:58andres az
February 26, 2026 AT 22:14