Surgical Options: When Procedures Beat Pills for Health
When medications don’t cut it, surgical options, medical procedures designed to fix or remove underlying problems in the body. Also known as interventions, they’re often the only way to stop pain, restore function, or save a life. Think of them as the body’s reset button—no more guessing if a pill will work, just a direct fix. They’re not always the first choice, but when they’re needed, they change everything.
Many people avoid surgery out of fear, but modern minimally invasive surgery, techniques that use small incisions and specialized tools to reduce trauma. Also known as keyhole surgery, it means less downtime, less scarring, and faster recovery. You don’t need a huge cut to fix a hernia, remove a gallbladder, or relieve spinal pressure. Even heart procedures now happen through tiny access points. These aren’t sci-fi—they’re everyday tools doctors use when drugs fail.
What makes surgical options powerful is how they fit into bigger treatment plans. For example, someone with severe arthritis might try painkillers for years, but when the joint wears out, a knee replacement isn’t extreme—it’s practical. Same with diabetes: if pills and insulin can’t control blood sugar, a gastric bypass might be the key to long-term health. Or consider prostate issues—meds help some, but for others, a simple procedure removes the blockage for good. These aren’t last resorts. They’re smart next steps.
Not every surgery is major. Some are quick, outpatient fixes—like removing a benign growth, clearing a blocked artery with a stent, or repairing a torn ligament. Others, like organ transplants or tumor removals, are complex and require careful planning. The common thread? They all target the root cause, not just the symptom. That’s why they show up in posts about ED meds, diabetes, and even cancer drugs—you’ll see people comparing pills to procedures because sometimes, one works better than the other.
You’ll find real comparisons here: when a drug like sildenafil helps erectile dysfunction, but surgery might be better for someone with physical blockages. Or how removing part of the stomach can be more effective than lifelong diabetes meds. These aren’t abstract ideas—they’re decisions real people make after weighing risks, costs, and outcomes. And in every case, the goal is the same: get you back to living, not just managing.
Recovery matters too. Surgical options aren’t just about the cut—they’re about what comes after. Physical therapy, diet changes, follow-up care—these are part of the deal. That’s why posts on bone health, heart failure, and even scar treatment for kids tie in. Surgery doesn’t end in the operating room. It’s the start of a new routine, and knowing what to expect makes all the difference.
So if you’re wondering whether to stick with pills or consider something more direct, you’re not alone. The posts below break down real cases, compare outcomes, and show you what works—not just what’s advertised. No fluff. Just facts, stories, and practical advice from people who’ve been there.
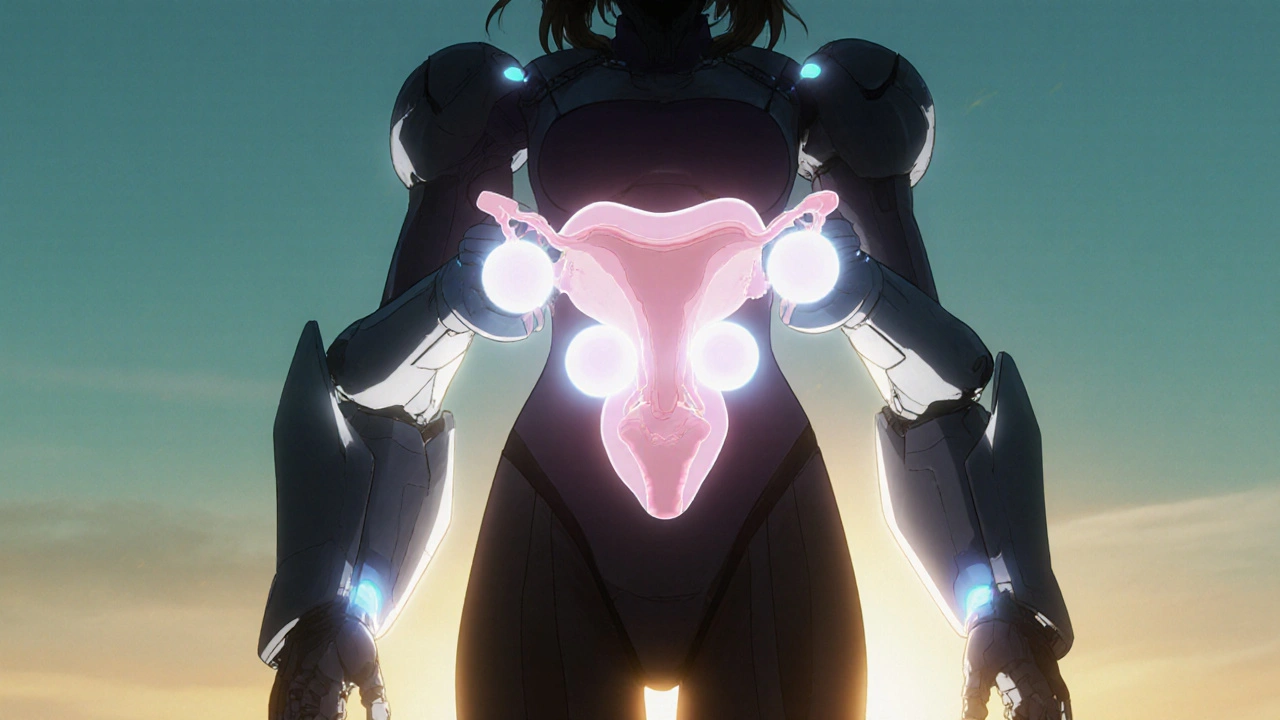
How Vaginal Surgery Treats Pelvic Organ Prolapse - Benefits, Risks, and Options
Explore how vaginal surgery treats pelvic organ prolapse, from native‑tissue repairs to mesh and apical suspensions, with risks, recovery tips, and future trends.