Polypharmacy and Side Effects: How Taking Too Many Medications Raises Your Risk
 Dec, 30 2025
Dec, 30 2025
Polypharmacy Risk Assessment Tool
How This Tool Works
This tool helps you identify potential risks in your medication regimen. Based on your input, it evaluates your risk level, highlights potentially unnecessary medications, and identifies common drug interactions. Always discuss these results with your doctor.
Your Risk Assessment
Risk Score
0
Low Risk
Higher scores indicate greater potential risk
Key Findings
Common Risks Detected
Based on your input, it's recommended to discuss with your doctor whether any medications could be safely reduced or stopped. This process is called deprescribing and can significantly reduce side effects and improve quality of life.
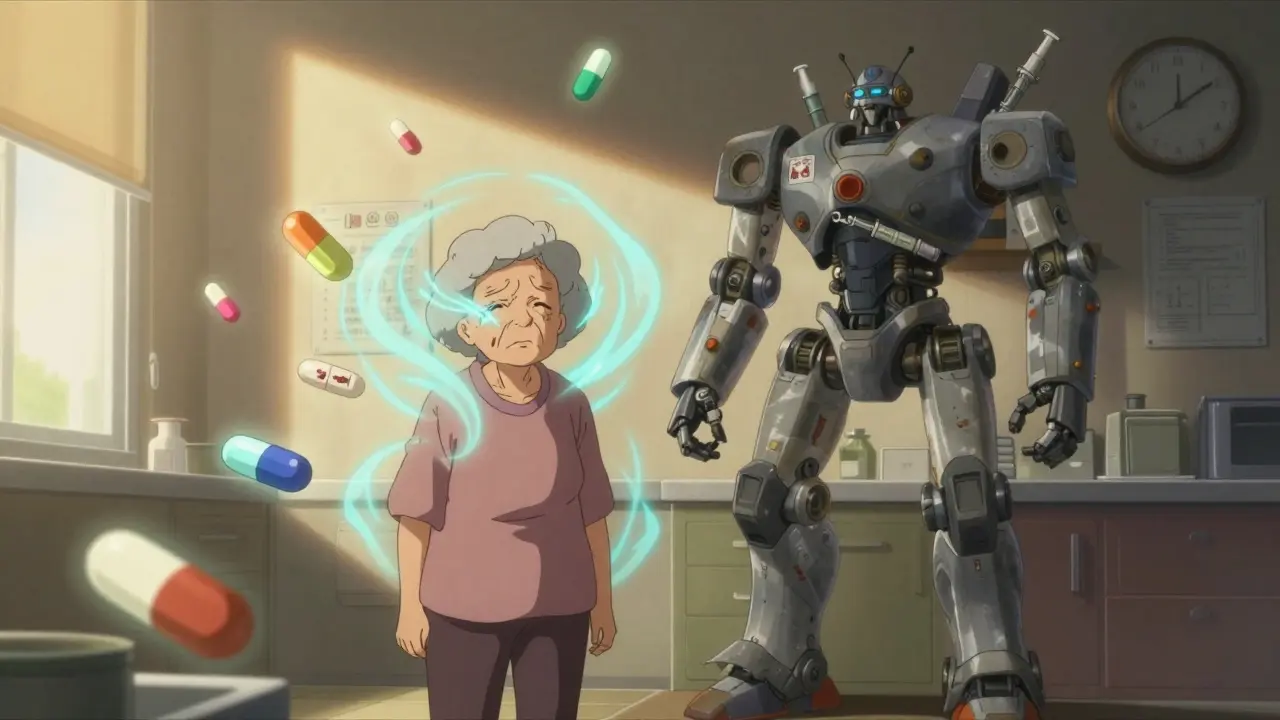
Imagine waking up every morning to a table full of pills - 10, 12, even 17 different ones. You take them with water, coffee, juice, whatever’s handy. Some are for your blood pressure. Others for arthritis, cholesterol, sleep, acid reflux, depression. You’ve been on this routine for years. But lately, you’ve been dizzy. Your memory’s slipping. You’re falling more often. You’re skipping doses because it’s just too much. And you’re not alone.
More than 40% of adults over 65 in the U.S. are taking five or more prescription drugs regularly. That’s polypharmacy. And while some of these medications are essential, many aren’t. The problem isn’t just the number - it’s how they interact, how your body changes with age, and how easily side effects get mistaken for new diseases.
What Exactly Is Polypharmacy?
Polypharmacy isn’t just having a lot of pills. It’s taking five or more medications at the same time, regularly. The number five is used as a red flag, not a rule. Some people need five meds because they have heart failure, diabetes, and kidney disease - and those drugs save their lives. That’s appropriate polypharmacy. But for many, it’s unnecessary. Maybe one drug treats a side effect of another. Maybe a doctor prescribed something years ago and never checked if it was still needed. That’s inappropriate polypharmacy - and it’s dangerous.
The World Health Organization calls it a major public health issue. Why? Because each extra pill adds risk. A 2016 study in BMJ Open found people taking 10 or more medications had a 28% higher chance of dying within a few years than those on just one to four. That’s not a small bump. That’s a sharp climb.
How Do Multiple Medications Cause Harm?
Your body doesn’t handle drugs the same way when you’re 75 as it did when you were 45. Your liver and kidneys slow down. Your brain becomes more sensitive. Even small doses can hit harder. And when you mix drugs, the risks multiply.
One common problem is drug interactions. If you’re on a blood thinner like warfarin and also take an over-the-counter painkiller like ibuprofen, you could start bleeding internally without noticing. Or if you’re taking an antihistamine for allergies and a sleeping pill, both can cause drowsiness - together, they can make you so dizzy you fall. A 2018 study from the Institute for Safe Medication Practices found that half of people on five or more drugs had at least one dangerous interaction.
Then there’s the medication cascade. This happens when a side effect gets misdiagnosed as a new condition. Say you take a blood pressure pill and get dizzy. Your doctor prescribes a balance medication. That makes you sleepy. Now you’re given a stimulant. Then you get constipation, so you’re given a laxative. Suddenly, you’re on eight drugs for one original problem. A 2019 JAMA Internal Medicine study found that 30-40% of unnecessary prescriptions come from these cascades.
Real People, Real Consequences
Martha, 72, from Ohio, was taking 17 pills a day. She couldn’t remember which ones she’d taken. She felt like a pharmacy on legs. After a medication review, three were stopped - her dizziness vanished. Robert, 68, was choosing between buying his heart medication or food. His monthly drug bill was $400. He didn’t have a choice.
On Reddit, a nurse shared a case of a 78-year-old on 12 medications. He was confused, falling, and barely eating. After removing three that weren’t helping, his energy returned. He started walking again. Another user, a pharmacist, said 60% of his senior patients skip doses because the regimen is too complex.
Medicare’s 2022 survey found 48% of people on five or more drugs believed at least one side effect was caused by their meds. Nearly 30% said they stopped going out because of how they felt.

Why Older Adults Are at Highest Risk
People over 65 are the most affected. Why? Because they’re the most likely to have multiple chronic conditions. But it’s not just the number of diseases - it’s how aging changes the body. Your liver can’t break down drugs as fast. Your kidneys flush them out slower. Your brain becomes more sensitive to sedatives, anticholinergics, and opioids.
The American Geriatrics Society says 91% of all adverse drug events in seniors are linked to polypharmacy. That’s not a coincidence. It’s a pattern. Drugs like benzodiazepines (for anxiety or sleep), NSAIDs (like ibuprofen), and anticholinergics (for overactive bladder or allergies) are especially risky. These are the top three culprits in inappropriate prescribing.
And here’s the kicker: many of these drugs were prescribed years ago. No one ever went back to ask if they were still needed.
What Can Be Done? Deprescribing Works
The solution isn’t stopping all meds. It’s stopping the ones that aren’t helping - or are hurting. That’s called deprescribing. It’s not about cutting corners. It’s about cleaning up.
A 2020 study in Annals of Internal Medicine found that a thorough medication review takes 25-40 minutes. That’s longer than most doctor visits. But it’s worth it. Medication reconciliation - writing down every single thing you take, including supplements and OTC drugs - reduces adverse events by 30%.
The American Geriatrics Society recommends annual reviews for anyone on five or more drugs. During these reviews, doctors should check:
- Is this drug still needed?
- Is it still working?
- Could it be causing side effects?
- Is there a safer alternative?
- Can it be lowered or stopped?
Tools like the Beers Criteria help doctors spot risky drugs for older adults. And new tech like MedWise, approved by the FDA in 2022, flags dangerous combinations before they’re prescribed. In one 2023 study, it cut high-risk drug pairs by 37%.

Cost and Convenience Are Huge Barriers
Even when doctors want to help, patients often resist. Why? Fear. They think stopping a drug means their condition will get worse. Or they’ve been told for years, “Take this every day.”
Cost is another big reason people don’t take their meds - or take too many. The average monthly cost for someone on five to nine drugs is $317. For those on 10 or more, it’s over $5,200 a year. That’s more than most people’s monthly rent. No wonder 65% of patients on 10+ drugs say cost makes them skip doses.
Complexity is just as bad. A 2021 study found patients on 10+ medications were 3.2 times more likely to miss doses than those on just one to four. The reasons? Too many pills, too many times a day, confusing instructions.
What You Can Do Right Now
You don’t need to wait for your doctor to bring it up. Start now:
- Make a full list of everything you take - prescriptions, OTC meds, vitamins, herbs, supplements. Don’t leave anything out.
- Bring that list to your next appointment. Ask: “Which of these are still necessary?”
- Ask about one drug at a time: “Can this be lowered? Stopped? Replaced?”
- If you’re feeling off - dizzy, tired, confused - ask: “Could this be a side effect?”
- Use a pill organizer. But don’t just fill it - review it monthly with a family member or pharmacist.
Don’t stop a drug on your own. But do start the conversation. Many side effects disappear once unnecessary drugs are removed.
The Bigger Picture
Polypharmacy isn’t just a personal problem. It’s a system failure. The U.S. spends $300 billion a year on avoidable costs from inappropriate medication use. Hospitals see 24% more admissions. Emergency visits jump 32%. And yet, only 12% of medical schools teach proper polypharmacy management.
Regulations are starting to catch up. Medicare now requires reviews for people on eight or more drugs. The SUPPORT Act mandates better care coordination. But real change needs more - better training for doctors, more time for patient reviews, and a culture that values simplicity over quantity.
The goal isn’t to take fewer drugs. It’s to take the right ones. And sometimes, the best medicine is no medicine at all.
Is polypharmacy always dangerous?
No. Polypharmacy isn’t automatically bad. For someone with heart disease, diabetes, and high blood pressure, taking four or five proven medications can cut their risk of death in half. The danger comes when medications are unnecessary, duplicated, or no longer helpful. The key is whether each drug is still doing its job - not how many you’re taking.
Can I stop a medication on my own if I think it’s causing side effects?
Never stop a prescribed medication without talking to your doctor first. Some drugs, like blood pressure or antidepressant meds, can cause serious withdrawal symptoms if stopped suddenly. But you can and should tell your doctor about any new side effects. They can help you safely reduce or replace the drug.
What are the most dangerous drugs for older adults?
The American Geriatrics Society’s Beers Criteria lists several high-risk drugs for seniors. These include benzodiazepines (like Valium or Xanax), anticholinergics (like diphenhydramine in Benadryl), NSAIDs (like ibuprofen), and certain sleep aids. These drugs can cause falls, confusion, memory loss, and kidney damage - especially when taken long-term or in combination.
How often should I get a medication review?
If you’re taking five or more medications, you should have a full review at least once a year. If you’ve recently been hospitalized, had a major health change, or started seeing new side effects, get reviewed sooner. Don’t wait for your doctor to bring it up - ask for it.
Does taking supplements count as polypharmacy?
Yes. Supplements like vitamin D, fish oil, ginkgo, or herbal remedies are still drugs in your body. They can interact with prescriptions, cause side effects, or be completely unnecessary. Many people don’t tell their doctors about supplements - but you should. A 2022 study found nearly 40% of seniors on multiple prescriptions were also taking supplements that had no proven benefit.
Hayley Ash
December 31, 2025 AT 12:07So let me get this straight - we're celebrating a 28% higher death rate as if it's a feature not a bug? My grandma took 14 pills and died quietly at 89. Maybe she just got tired of the circus
kelly tracy
December 31, 2025 AT 19:22Deprescribing is just lazy medicine. If you can't afford your meds, don't take them. If you're dizzy, maybe you're just old. Stop pretending pharmaceuticals are the enemy. Your body's supposed to break down. That's biology, not a system failure.
Kelly Gerrard
January 2, 2026 AT 11:09I appreciate the thoroughness of this post. The data presented is compelling and aligns with clinical observations in geriatric populations. However, the emphasis on reduction without adequate consideration of patient autonomy and individualized risk-benefit profiles may inadvertently undermine trust in physician judgment. Medication regimens are not arbitrary; they are the result of iterative clinical decision-making under complex comorbid conditions.
Aayush Khandelwal
January 3, 2026 AT 18:40Look, polypharmacy isn't the villain - it's the symptom. The real pathology is the fragmented healthcare ecosystem where cardiologists, neurologists, endocrinologists, and psychiatrists all write scripts like they're playing Jenga with your life. No one's talking to each other. No one's looking at the whole damn tower. We need integrated care teams, not siloed specialists with their own little kingdoms. And yes, supplements count - that turmeric capsule you think is 'natural' is a CYP3A4 inhibitor that'll mess with your statin like a drunk intern in the ER.
Sandeep Mishra
January 3, 2026 AT 21:31Been there. My dad was on 11 pills. Dizzy, confused, stopped eating. We did the review - cut three. He started laughing again. Walked to the mailbox. Told me stories about his childhood. That's not a win for medicine. That's a win for common sense. You don't need more drugs to live well. You need fewer distractions from being alive.
Joseph Corry
January 4, 2026 AT 01:11It's fascinating how this piece romanticizes simplicity as virtue. The assumption that fewer drugs equate to better health is a neoliberal fantasy. The body is not a machine that can be tuned down. Aging is a cascade of physiological decay. To deprescribe is to surrender to entropy. The real tragedy isn't polypharmacy - it's that we're still pretending medicine can reverse the inevitable. We're not treating disease anymore. We're just delaying the funeral with a cocktail of chemical band-aids.
srishti Jain
January 5, 2026 AT 09:06My aunt took 17 pills. She forgot which ones were for what. One day she took 4 blood pressure pills by accident. Ended up in the ER. No one asked her if she needed all of them. Just kept adding more. Classic.
Colin L
January 6, 2026 AT 21:21You think this is bad? Try living in a nursing home where they give you a whole damn pharmacy every morning just to keep you quiet. I work in geriatrics. I've seen people on 20+ meds because it's easier than talking to them. They're not sick from disease - they're sick from bureaucracy. The system doesn't care if you're dazed or falling. It cares if the billing code gets submitted. I had a patient on gabapentin, amitriptyline, melatonin, zolpidem, lisinopril, atorvastatin, metformin, levothyroxine, omeprazole, hydrochlorothiazide, calcium, vitamin D, aspirin, celecoxib, and a 'memory support' supplement that was just sugar and saw palmetto. That's not medicine. That's a vending machine with a stethoscope. And you know what? The doctor who prescribed all that? He retired last year. Left it to someone else to clean up. We don't fix systems. We just pass the bag of pills.
Cheyenne Sims
January 7, 2026 AT 15:22While the concerns regarding polypharmacy are valid, the underlying premise that American healthcare is uniquely flawed is misleading. In the United Kingdom, the National Health Service mandates comprehensive medication reviews for elderly patients with five or more prescriptions. The British model demonstrates that centralized oversight, standardized protocols, and physician accountability can mitigate these risks without resorting to alarmist rhetoric. The American system, while imperfect, benefits from innovation, regulatory oversight, and technological advancements such as MedWise, which are not universally available abroad. To dismiss the efficacy of modern pharmacotherapy is to ignore decades of clinical progress.