Pediatric Antihistamine Dosing Errors: How to Prevent Dangerous Side Effects
 Dec, 10 2025
Dec, 10 2025
Pediatric Antihistamine Dosing Calculator
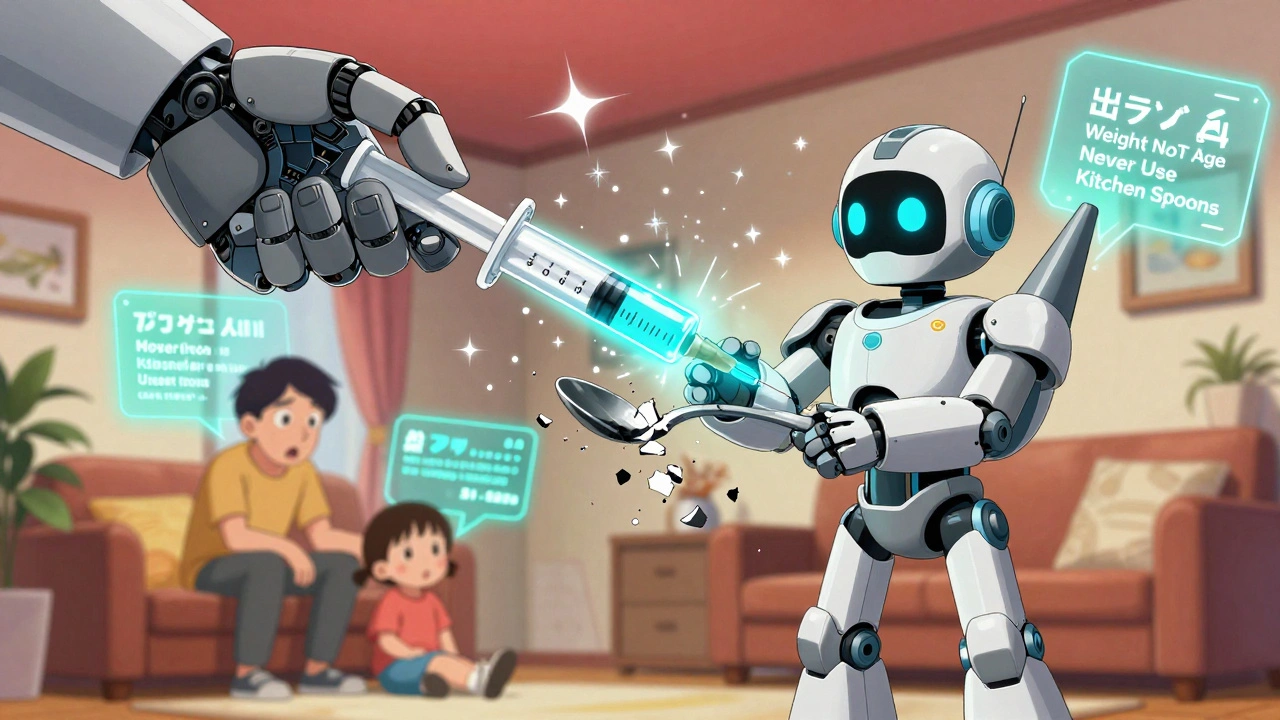
How to Use This Calculator
This tool calculates accurate pediatric antihistamine doses based on your child's weight. Always use a proper measuring device (oral syringe) and follow dosage guidelines for safety.
- Use weight-based dosing, not age-based
- Second-generation antihistamines (Claritin, Zyrtec) are safer
- Never use kitchen spoons for dosing
Dosing Results
Every year, thousands of children end up in emergency rooms because someone gave them the wrong dose of an antihistamine. Not because the medicine is dangerous - but because the dose was wrong. A teaspoon instead of a milliliter. An adult pill instead of a child’s liquid. A guess based on age instead of weight. These aren’t rare mistakes. They’re common, preventable, and sometimes life-threatening.
Why Kids Are at Risk
Children aren’t just small adults. Their bodies process medicine differently. A dose that’s safe for a 150-pound adult can be toxic for a 20-pound toddler. First-generation antihistamines like diphenhydramine (Benadryl) are especially risky. They cross the blood-brain barrier easily, causing drowsiness, confusion, and in high doses, seizures or breathing problems. The FDA and American Academy of Pediatrics warn against using them for colds or routine allergies in kids under 2. Yet, they’re still widely available - and often misused.Second-generation antihistamines like loratadine (Claritin) and cetirizine (Zyrtec) are safer. They’re less likely to cause drowsiness and have a much wider safety margin. But even these can cause harm if dosed incorrectly. The problem isn’t the drug - it’s the measurement.
The Measurement Mistake That Kills
Kitchen spoons are the #1 cause of dosing errors. A teaspoon from your drawer might hold 4 mL. Or 7 mL. Or even 2.5 mL. That’s a 300% difference in dose. A 2021 study in Pediatrics found that 42% of parents still use kitchen spoons to give liquid medicine. One parent gives their 22-pound child ¾ teaspoon of Benadryl thinking it’s safe. But if their spoon holds 7 mL instead of 5 mL, they’ve given nearly 17 mg instead of 9.3 mg - almost 80% too much.Even the labels can trick you. Children’s Benadryl liquid is 12.5 mg per 5 mL. That’s 2.5 mg per mL. Children’s Zyrtec is 1 mg per mL. So 2.5 mL of Zyrtec equals 2.5 mg. But 2.5 mL of Benadryl equals 6.25 mg. They look the same. They’re both clear liquids. But they’re not the same. Confusing them can lead to overdose.
What the Numbers Really Mean
Here’s what you need to know about common pediatric antihistamines:- Diphenhydramine (Benadryl): 12.5 mg per 5 mL liquid. Chewable tablets: 12.5 mg. Adult tablets: 25 mg or 50 mg. Never give adult tablets to a child.
- Loratadine (Claritin): Children’s liquid is 5 mg per 5 mL. One teaspoon (5 mL) = 5 mg. For kids 1-2 years old: 2.5 mg (half a teaspoon). For 2-5 years: 5 mg once daily.
- Cetirizine (Zyrtec): Children’s liquid is 1 mg per mL. For kids 2-5 years: 2.5 mg (2.5 mL). For 6-11 years: 5 mg (5 mL).
Weight matters more than age. A 30-pound child might need the same dose as a 5-year-old who weighs 40 pounds. Always check the weight-based chart on the bottle - not the age chart. If the bottle doesn’t have one, ask your pharmacist or doctor for it.
Why First-Generation Antihistamines Should Be Avoided
Diphenhydramine has a narrow therapeutic window - the difference between a helpful dose and a dangerous one is small. Studies show its toxic dose is only about twice the therapeutic dose. For cetirizine, it’s ten times higher. That’s why 83% of emergency visits for antihistamine overdoses involve Benadryl, even though it’s used less often than Claritin or Zyrtec.It’s also sedating. Parents sometimes give it to help kids sleep - especially during colds. But that’s not its purpose. The American College of Allergy, Asthma, and Immunology found that 67% of pediatricians see parents using Benadryl for cold symptoms in kids under 2 - a practice that’s not only ineffective but risky. The European Medicines Agency has banned its use in children under 2. The FDA and AAP agree: don’t use it for routine allergies or colds in young kids.
How to Measure Correctly - Every Time
Forget spoons. Forget cups. Use an oral syringe. The kind that comes with the medicine. If it didn’t come with one, go buy one - they’re $2 at any pharmacy. Make sure it’s marked in milliliters (mL), not teaspoons.Here’s how to do it right:
- Read the label. Know the concentration (mg/mL).
- Know your child’s weight in pounds or kilograms.
- Use the weight-based chart on the bottle or from your doctor.
- Draw up the exact amount in the syringe. Don’t guess.
- Give the medicine slowly into the side of the mouth, not straight down the throat.
- Don’t re-dose if your child spits it out. Call your pediatrician.
Use the same syringe for every dose. Don’t switch between different medicines with the same device - even if you rinse it. Residue adds up. A 2021 Consumer Reports analysis found 44% of dosing errors happened because parents reused measuring tools across multiple medications.
What to Do If You’re Not Sure
If you’re confused - pause. Don’t guess.Call Poison Control at 1-800-222-1222. They’re available 24/7. They’ve handled over 31% of all antihistamine-related calls - and they know exactly what to do. You don’t need to wait for symptoms. If you think you gave too much, call immediately.
Use the Poison Control app. It has a built-in dosing calculator. Just enter your child’s weight, the medicine, and the dose. It tells you if it’s safe. It’s free, reliable, and used by over 1.2 million families.
Ask your pharmacist. They’re trained to catch dosing errors. One study found pharmacists catch 19% of pediatric antihistamine prescriptions before they’re filled - usually because someone wrote “Benadryl 12.5 mg” without specifying it was the children’s liquid.
What’s Changing - And What’s Working
Hospitals and clinics are getting better. Most now use electronic health records that flag weight-based dosing errors. If a parent enters a 15-pound child and tries to order 25 mg of Benadryl, the system alerts the doctor. That’s cut calculation errors by 76%.Some pharmacies now offer color-coded dosing charts based on weight. The “Dose Right” program, used in nearly half of U.S. pediatric clinics, gives parents a chart specific to their child’s weight - no math needed. Just match the color.
The FDA is testing QR codes on medicine labels that link to short videos showing how to use the syringe. A pilot at Boston Children’s Hospital showed a 53% drop in dosing errors.
But the biggest change? More parents are choosing second-generation antihistamines. In 2010, only 42% of pediatric antihistamine use was for loratadine or cetirizine. Now it’s 68%. That’s because they’re safer, simpler, and don’t cause drowsiness.
Real Stories, Real Risks
One mother gave her 23-month-old daughter a 50 mg adult Benadryl tablet, thinking it was the children’s version. The child was hospitalized for 48 hours with respiratory distress. That’s case #15678231 in the FDA’s database.A grandmother in Ohio gave her 18-month-old grandson 10 mL of Benadryl because the bottle said “1 tsp” - and she thought a teaspoon was a big spoon. The child had a seizure. He recovered, but the trauma lasted for months.
On Reddit, a parent wrote: “I gave my 22lb 18-month-old the 1-2 year dose of Zyrtec, but the Benadryl chart said ¾ tsp. Are these the same? I’m terrified I’m poisoning my child.” The answer? No. They’re not the same. And that fear? It’s real. And it’s valid.
What You Can Do Today
1. Throw out your kitchen spoons for medicine. Buy a syringe. 2. Check the concentration on every bottle. Write it down if you need to. 3. Use weight, not age - always. 4. Choose Claritin or Zyrtec over Benadryl for routine allergies. 5. Save Poison Control’s number in your phone. And your partner’s phone. 6. Teach-back: Have another adult watch you measure the dose. If they nod, you’re doing it right.Medicine isn’t guesswork. It’s science. And for kids, getting it right isn’t optional - it’s lifesaving.
john damon
December 11, 2025 AT 08:04matthew dendle
December 11, 2025 AT 21:28Monica Evan
December 12, 2025 AT 19:52Taylor Dressler
December 13, 2025 AT 02:47Aidan Stacey
December 14, 2025 AT 11:40Jean Claude de La Ronde
December 15, 2025 AT 21:11Jim Irish
December 15, 2025 AT 23:17Mia Kingsley
December 16, 2025 AT 09:01Katherine Liu-Bevan
December 16, 2025 AT 18:17Courtney Blake
December 18, 2025 AT 15:00Kristi Pope
December 20, 2025 AT 05:44Eddie Bennett
December 20, 2025 AT 22:22