Can Probiotics Prevent Cystitis? Evidence, Strains, and How to Use Them
 Oct, 12 2025
Oct, 12 2025
Probiotic Strain Comparison for Cystitis Prevention
Select a probiotic strain to see detailed information about its effectiveness for preventing cystitis. This tool compares key metrics including evidence level, recommended dosage, and administration route based on the latest research.
Step 1: Click on a probiotic strain to see its detailed profile. Step 2: Review the evidence, dosage, and administration route. Step 3: Consider your personal situation and select the strain that best fits your needs. Step 4: Consult your healthcare provider before starting any new supplement regimen.
| Probiotic Strain | Dosage (CFU/day) | Evidence Level | Preferred Route | Benefits |
|---|---|---|---|---|
| Lactobacillus crispatus | 10-20 billion | High (multiple RCTs) | Vaginal suppository or oral capsule | Strong evidence for cystitis prevention, especially when administered vaginally |
| Lactobacillus rhamnosus GR-1 | 5-10 billion | Moderate (5+ trials) | Oral capsule | Good evidence for cystitis prevention, convenient oral administration |
| Lactobacillus reuteri RC-14 | 5-15 billion | Moderate (2 RCTs) | Vaginal tablet | Effective when administered vaginally, good option for recurrent cystitis |
| Bifidobacterium lactis | 5-10 billion | Low (observational) | Oral capsule | Moderate evidence, may support general urinary health |
Select a probiotic strain to see detailed information
This tool helps you compare key characteristics of different probiotic strains shown in the article for cystitis prevention. Consider dosage, administration route, and evidence level when making your selection.
Many wonder if probiotics can help prevent cystitis. The short answer is: there is growing scientific backing, but the picture isn’t black‑and‑white. Below we break down what cystitis is, why the body’s microbes matter, which probiotic strains show promise, and how to add them safely into your routine.
What Is Cystitis?
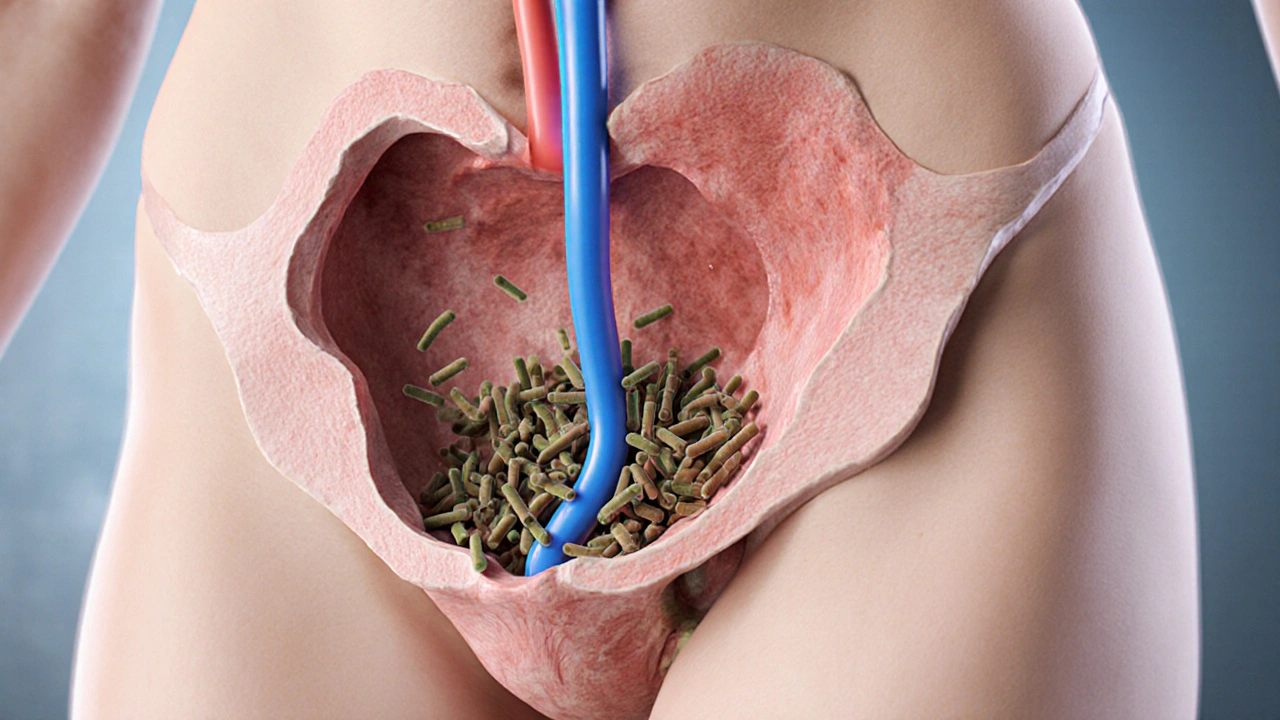
Cystitis is an inflammation of the bladder wall, most often caused by bacterial infection. When bacteria travel up the urethra and colonise the bladder, they irritate the lining, leading to burning during urination, frequent urges, and sometimes blood in the urine. In medical terminology, cystitis falls under the broader umbrella of urinary tract infection (UTI), which includes infections of the kidneys, ureters, and urethra as well.
Women are disproportionately affected because of a shorter urethra and its proximity to the vagina and anus. Roughly 50-60% of women will experience at least one UTI in their lifetime, and many report recurrent episodes.
How the Urinary and Vaginal Microbiome Influence Cystitis
The human body hosts trillions of microbes, and the balance between friendly and harmful species plays a decisive role in bladder health. The vaginal microbiome is typically dominated by Lactobacillus species, which produce lactic acid and keep the local pH low. This acidic environment is hostile toEscherichia coli (E.coli), the bacterium responsible for about 70-95% of uncomplicated cystitis cases.
When the Lactobacillus population wanes-due to antibiotics, hormonal changes, or sugary diets-E.coli can flourish and migrate up the urethra. Restoring a healthy community of beneficial bacteria is therefore a logical step toward prevention.

Do Probiotics Really Reduce Cystitis Risk?
Research over the past decade has moved beyond anecdote to controlled trials. A 2022 systematic review of 12 randomised studies found that women who took probiotic supplements containing Lactobacillus crispatus or Lactobacillus rhamnosus experienced a 30‑40% lower recurrence rate compared with placebo. The effect was strongest when the probiotic was taken for at least three months and combined with standard hygiene advice.
Another trial in 2023 focused on oral versus vaginal administration of Lactobacillus reuteri. Vaginal tablets reduced recurrence by 45% while oral capsules achieved a 20% reduction, suggesting that delivering the bacteria close to the infection site may boost efficacy.
While not every study shows a dramatic benefit, the overall trend points to a modest but statistically significant protective effect-especially for women with a history of recurrent cystitis.
Best Probiotic Strains and Dosage Recommendations
| Strain | Typical Daily Dose (CFU) | Evidence Level | Preferred Route |
|---|---|---|---|
| Lactobacillus crispatus | 10-20billion | High (multiple RCTs) | Vaginal suppository or oral capsule |
| Lactobacillus rhamnosus GR-1 | 5-10billion | Moderate (5+ trials) | Oral capsule |
| Lactobacillus reuteri RC-14 | 5-15billion | Moderate (2 RCTs) | Vaginal tablet |
| Bifidobacterium lactis | 5-10billion | Low (observational) | Oral capsule |
Key take‑aways:
- Choose a product that lists the exact strain name (e.g., L.crispatus ATCC33820). The strain matters more than the species.
- Look for a dose of at least 5billion colony‑forming units (CFU) per day; higher doses have not shown extra benefit and may increase cost.
- If you’re comfortable with vaginal administration, a suppository or tablet placed once nightly for three weeks can seed the local microbiome more directly.
How to Incorporate Probiotics Into Your Daily Routine
Below is a practical, step‑by‑step plan that blends the science with everyday life.
- Pick the right product. Opt for a reputable brand that guarantees live organisms through the expiration date and stores the product in a cool, dry place.
- Start with a loading phase: take the recommended dose every day for the first 2-4 weeks. This gives the beneficial bacteria a chance to colonise.
- Maintain a maintenance phase: after colonisation, you can reduce to 3-5days a week, especially during high‑risk periods (e.g., after sexual activity, during menstruation, or when on a course of antibiotics).
- Pair with prebiotic foods. Fiber‑rich foods like bananas, oats, and chicory root feed the probiotic strains and improve their survivability.
- Stay hydrated. Drinking at least 2litres of water daily helps flush out any stray bacteria that might try to ascend the urinary tract.
- Practice good hygiene: urinate shortly after intercourse, avoid douches, and wipe front‑to‑back.
If you’re prescribed antibiotics for a cystitis episode, start the probiotic at least two hours after the antibiotic dose and continue for at least a week post‑treatment to help restore microbial balance.

Safety, Side Effects, and Who Should Be Cautious
Probiotics are generally safe for healthy adults. Mild side effects such as gas, bloating, or a temporary increase in bowel movements can occur during the initial loading phase. These usually resolve within a week.
People who should consult a healthcare provider before starting include:
- Those with compromised immune systems (e.g., organ transplant recipients, chemotherapy patients).
- Individuals with central venous catheters or recent major surgery.
- Pregnant or breastfeeding women, although many studies report no adverse outcomes, professional guidance is advisable.
In rare cases, probiotic bacteria have been isolated from blood cultures in severely immunocompromised patients. While the risk is minuscule for the average person, it underscores the need for medical advice when underlying conditions exist.
Quick Checklist: Probiotic‑Ready Prevention of Cystitis
- Identify a high‑quality probiotic containing L.crispatus or L.rhamnosus GR‑1.
- Commit to a 4‑week loading phase (10-20billion CFU daily).
- Combine with prebiotic foods and at least 2L of water per day.
- Practice post‑coital urination and proper wiping technique.
- Re‑evaluate after 3 months; if recurrent infections persist, discuss further evaluation with a clinician.
Frequently Asked Questions
Can I get probiotics from food instead of a supplement?
Yes. Yogurt with live cultures, kefir, and fermented vegetables contain Lactobacillus strains, but the specific strains studied for cystitis (like L.crispatus) are rarely present in food. A targeted supplement ensures you get the right dose and strain.
How long does it take to see a protective effect?
Most trials report a noticeable reduction in recurrence after 8-12 weeks of consistent use. Benefits tend to plateau, so continuing a maintenance dose is recommended for ongoing protection.
Will probiotics interfere with antibiotics used to treat cystitis?
Take the probiotic at least two hours apart from the antibiotic dose. This timing minimises the chance that the antibiotic kills the beneficial bacteria, allowing the probiotic to survive and colonise after the antibiotic course ends.
Are there any probiotic brands that are clinically validated?
Brands that have published peer‑reviewed studies-such as Vivomixx®, Urovir®, and Culturelle® for women-list the exact strains used in trials. Look for a clear label showing strain identification and CFU count.
Can men benefit from probiotics to prevent bladder infections?
Men experience cystitis less frequently, but the same microbiome principles apply. Some studies suggest that Lactobacillus‑based probiotics can reduce the incidence of recurrent UTIs in men, especially after catheter use.
Andy V
October 12, 2025 AT 18:41Wow, that was a sloppy typo fest.
mathokozo mbuzi
October 13, 2025 AT 09:58The overview of probiotic strains is clear, but remember that individual microbiomes vary widely, so results can differ from person to person.
When choosing a product, prioritize those that explicitly list the strain identifier, because generic Lactobacillus labels can be misleading.
Also, consider your own health context-some people respond better to oral capsules while others benefit from vaginal suppositories.
Penny X
October 14, 2025 AT 01:15While supplementing with beneficial bacteria is commendable, it remains essential to consult a qualified clinician rather than self‑prescribing based on internet articles.
Neglecting professional guidance can lead to unintended consequences, especially for vulnerable populations.
Amy Aims
October 14, 2025 AT 16:31Great info! 🙌 If you’re thinking about trying a probiotic, start with the recommended loading phase and stay consistent-you’ll likely notice a difference in urinary comfort.
Keep up the good habits and remember hydration is your best friend! 😊
Shaik Basha
October 15, 2025 AT 07:48Yo, I tried the L‑crispatus supposytes after a rough UTI and felt the burn ease up fast.
Make sure you store ‘em cool, otherwise the live bugs die and you waste cash.
Also, don’t forget to chug water, ’cause the probiotics need a highway to get to the bladder.
Michael Ieradi
October 15, 2025 AT 23:05Interesting point, however, storing probiotics in a cool, dry place is indeed crucial; exposure to heat, moisture, or direct sunlight can significantly reduce viable CFU counts, thereby diminishing therapeutic efficacy.
Pat Mills
October 16, 2025 AT 14:21The United States has long been at the forefront of probiotic research, yet many citizens remain ill‑informed about the nuances of strain specificity.
Lactobacillus crispatus, for instance, has demonstrated a remarkable capacity to re‑establish a protective vaginal milieu when administered vaginally.
Its mechanism, primarily the production of D‑lactic acid, creates an environment hostile to uropathogenic Escherichia coli.
Nevertheless, the market is saturated with generic multi‑strain products that lack rigorous clinical validation.
Consumers are often misled by flashy packaging and inflated CFU claims that do not translate into clinical benefit.
Furthermore, the regulatory landscape permits manufacturers to label products with vague strain names, obscuring true identity.
A diligent practitioner will scrutinize batch testing data, ensuring that the stated strain matches the genetic profile used in peer‑reviewed trials.
Clinical outcomes improve dramatically when patients adhere to a minimum four‑week loading regimen, as opposed to sporadic use.
Hydration, dietary prebiotics, and avoidance of unnecessary antibiotics synergize with probiotic therapy to maintain urinary health.
It is also worth noting that while oral capsules of L. rhamnosus GR‑1 are convenient, they achieve lower colonization rates in the vaginal niche than suppositories.
Patients who prioritize convenience may still benefit, but they should temper expectations regarding magnitude of effect.
Economic considerations cannot be ignored; high‑dose products often carry a premium price tag that may be prohibitive for low‑income individuals.
Equitable access to evidence‑based probiotic interventions should be a public health priority.
Healthcare providers must therefore educate patients not only about product selection but also about realistic timelines for observable improvement.
In summary, the science supports probiotic prophylaxis for recurrent cystitis, provided the correct strain, dosage, and administration route are employed.
Failure to respect these parameters reduces the intervention to a placebo and squanders both resources and confidence.
neethu Sreenivas
October 17, 2025 AT 05:38It’s fascinating how the vaginal microbiome acts as a frontline defense; the dominance of lactobacilli creates a low‑pH barrier that discourages pathogenic invasion. 🌿 When antibiotics disrupt this balance, probiotic re‑colonization can quickly restore resilience. 🦠 A balanced diet rich in prebiotic fibers further supports these beneficial microbes, offering a holistic approach to urinary health.
Matthew Ulvik
October 17, 2025 AT 20:55Exactly! Keep it simple: take the right probiotic daily, drink plenty of water, and eat foods like bananas and oats that feed the good bugs. 👍 Consistency is key, and you’ll feel the difference.
Dharmendra Singh
October 18, 2025 AT 12:11Absolutely, professional guidance is vital; many over‑the‑counter blends miss the mark on strain specificity and dosage, leading to mixed results. It is wise to ask a doctor or a trained pharmacist to verify that the product contains the clinically studied strain and appropriate CFU levels.
Rocco Abel
October 19, 2025 AT 03:28Some folks think big pharma suppresses probiotic research to protect their antibiotic profits, but the data is out there for anyone willing to dig. The key is to seek out peer‑reviewed studies and avoid marketing hype.
Dawn Mich
October 19, 2025 AT 18:45Don’t buy into every wild claim; the truth lies between the hype and the skepticism, and only rigorous trials can separate fact from fiction. Blind faith in any supplement without evidence is a recipe for disappointment.
charlise webster
October 20, 2025 AT 10:01While many tout probiotics as a panacea for cystitis, the evidence remains modest and not all strains are created equal, so blanket recommendations are premature.
lata Kide
October 21, 2025 AT 01:18Yo, you’re missing the drama! The moment you drop the right strain, it’s like a superhero squad invading the bladder, kicking E.coli to the curb! 🦸♀️💥 The science may be slow, but the results speak louder than any paper.
Mark Eddinger
October 21, 2025 AT 16:35When evaluating probiotic efficacy, it is essential to consider the study design, sample size, and statistical significance. Randomized controlled trials remain the gold standard for establishing causality.
Francisco Garcia
October 22, 2025 AT 07:51The recent meta‑analysis highlighted that Lactobacillus crispatus shows the most consistent reduction in recurrence rates, especially when administered vaginally, whereas oral formulations yield variable outcomes.
Patrick Renneker
October 22, 2025 AT 23:08In the realm of urinary tract infection prophylaxis, the role of probiotic supplementation warrants a nuanced appraisal, taking into account microbial ecology, host factors, and the pharmacokinetics of bacterial colonisation. The extant literature, while promising, exhibits heterogeneity in methodology, including disparate dosing regimens and divergent routes of administration. Accordingly, clinicians must exercise discernment when extrapolating trial results to individual patient scenarios. Moreover, the interplay between prebiotic dietary intake and probiotic viability underscores the necessity of a comprehensive therapeutic strategy. Ultimately, a judicious, evidence‑driven approach will optimise patient outcomes whilst mitigating undue reliance on unsubstantiated claims.
KAYLEE MCDONALD
October 23, 2025 AT 14:25Agreed-balanced, evidence‑driven use of probiotics can complement standard UTI prevention tactics.
Alec McCoy
October 24, 2025 AT 05:41Hey everyone, love the deep dive on strains! If you’re new to this, start with a reputable brand that lists the exact strain, because the difference between a generic Lactobacillus and a clinically studied L. crispatus is huge. Consistency is your secret weapon-take it every day for at least a month before you expect noticeable change. Pair it with plenty of water and some prebiotic foods like garlic and onions to feed those good microbes. And remember, if you ever get a full-blown infection, antibiotics are still the frontline-probiotics are a preventive sidekick, not a replacement. Keep tracking your symptoms, and you’ll soon see the pattern of improvement. Stay motivated and keep those bladders happy!
Aaron Perez
October 24, 2025 AT 20:58Indeed, the synergistic effect of hydration, prebiotic intake, and strain‑specific probiotic administration constitutes a multifactorial prophylactic regimen; neglecting any component undermines the holistic objective, thereby diminishing overall therapeutic efficacy.